- NURS FPX 8045 Assessment 6 Synthesis of Evidence Substantiating an Intervention.
Synthesis of Evidence Substantiating an Intervention
Closing the recognized practice gap is relevant for the enhancement of the given patients’ results and such a health care field. The practice gap mentioned in Assessment 4 is the major failure of healthcare professionals in a hospital to strictly follow protocols on hand hygiene. This has been associated with an increased incidence of HAIs that cause additional morbidity, mortality, and cost to the patients.
This is because improving patient safety and reducing the burden of HAIs is still inadequate, given the gap that is created (World Health Organization, 2020). To close this practice gap, I have decided to focus on investigating the effects of exanimation of a whole organism and assigning a hand hygiene training and monitoring program as the intervention.
It also involves planned educational sessions/ meetings, he/she observes compliance leveled on electronic sensors installed in different parts of the healthcare facility, and provides instant feedback to the healthcare workers. The above intervention has been selected because it can enhance the levels of hand hygiene through the provision of further education and positive feedback after identifying areas for improvement (McLaws, 2020).
Introduction that Provides an Overview of Your Gap in Practice, and Ends with a PICOT Question
Hand hygiene practices are known to be a vital measure in the prevention of infections among health care workers and other patients in hospitals. Even, though the literature has proven that proper hand hygiene is effective many healthcare providers fail to practice it, worsening HAIs.
These infections lead to longer hospitalization among patients, higher charges in healthcare expenses, and increased mortality rates. Healthcare Organizations should pay special attention to hand hygiene and other related precautions as one of the key strategies to preventing HAIs among patients.
To fill this gap, I have decided to study the effects of a hand hygiene training and monitoring program as the intervention. It consists of; training sessions, the use of electronic sensors to monitor the extent of hand hygiene caregiver’s adherence to the recommended standard of hygiene care at the point of care as well as giving the e- feedback to the caregivers.
The reason for choosing this intervention is founded on the assumption that it stands high chances of enhancing hand washing practices equally due to education and feedback practices which signify its reliability to enhance habits positively (McLaws, 2020). It has been established that long term training with feedback in compliance Monday can translate to long term improvements of hand hygiene and consequently lowering of HAIs (World Health Organization, 2020).
Five Recent Research Articles
In the article (McLaws,2020), it is discussed the correlation between the measures of hand hygiene practices and the rates of HAIs. The study demonstrates the productivity of training, which was held repeatedly, and the feedback received in enhancing Hand hygiene by HCW’s.
Therefore, the results presented in this article as well as the analysis of the barriers to compliance and the advantages of real-time monitoring and feedback provide evidence for the idea that the hand hygiene program should improve the adherence to guidelines and minimise HAIs.
(Alzyood et al. 2020) have stressed the significance of the hand in getting rid of illnesses, especially when concerning the COVID-19 situation. The study also explains how COVID-19 has brought the necessity of proper hand washing practices, thus approving the promotions of training and control programs meant to enhance compliance.
It is important to note that the authors maintain that constant education and feedback systems are key when it comes to the details of hand hygiene, jobs that ensure safety of not only patients but the health care personnel as well.
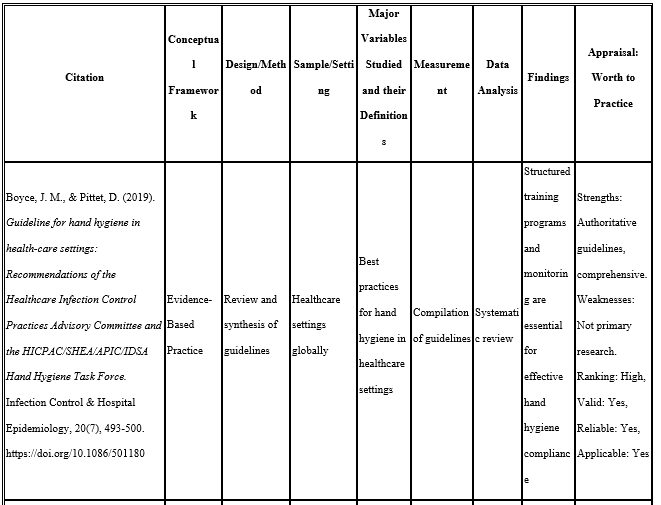
Adopted and labeled as the guideline for hand hygiene, Boyce and (Pittet’s, 2019) document contains extensive recommendations regarding the practices of hand hygiene in healthcare facilities. The guideline highlights the need to integrate and implement professional course and competencies in structure to improve compliance to hand hygiene.
Monitoring and feedback approaches are also underlined as the means of maintaining high levels of compliance. The objective of this article is to provide the necessary background for expanding hand hygiene promotion strategies in the clinical setting.
Critical Review of All Chosen Articles
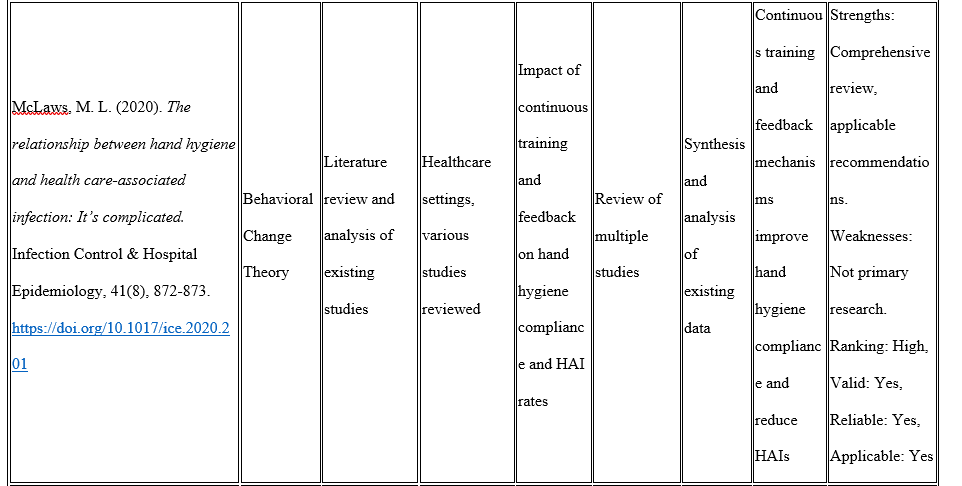
McLaws, M. L. (2020)
In her article, (McLaws, 2020) also underlines the importance of the staff training and the feedback in the process of enhancing the strict hand hygiene adherence as well as decreasing the HAIs rate. This research is therefore based on Behavioral Change Theory and uses a literature review and synthesis of the existing literature.
The first research question focused on understanding the effects of ongoing training and performa0ereviews on hand hygiene as well as the HAI incidence rates. Research evidence available reveals that the mechanisms increase the level of compliance and reduced infection incidences. This article was chosen for review because it offers a comprehensive literature review of different works and highlights such components of the proposed approach as training and feedback.
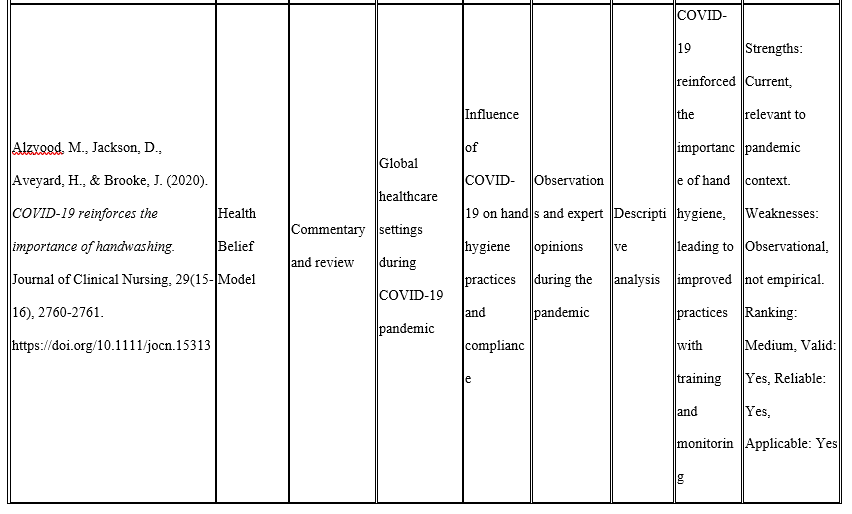
Alzyood, M, Jackson, D , Aveyard, H & Brooke, J 2020
(Alzyood et al, 2020) describe the COVID-19 pandemic situation and the remarks concerning the enhancement of hand hygiene promotion during the crisis. As quantitative research based on the Health Belief Model, this study employs the commentary and review approach to discuss hand hygiene during the COVID-19 pandemic around the world.
The important areas identified to be the subject of research include infection control, training, and monitoring influenced by COVID-19. The study’s results indicate that there is a positive outcome where the pandemic has been followed up with training as well as checking. This article was selected because it shows the failure of patients to institutionalize hand hygiene as a measure to prevent infections as a global health promotion strategy, which supports the argument for the need for broad, hand hygiene promotion.
Boyce, J. M. , & Pittet, D. ( 2019)
Contemporary epidemiology of nosocomial infections: lamp or spotlight for infection prevention? In B. M. et al Armstrong D. (Eds. ), The Darwinian imperative of nosocomial infections (pp. 53–64). Nova Biomedical Book Publishers. A guideline review has been done by Boyce and Pittet (2019) which discusses the right measures of hand hygiene in health care facilities.
The source of this evidence-based practice is compiled from guidelines or recommendations from different sources of authority. The main objective is healthcare workers’ proper hand hygiene actions, which include structured educational activities and related controls. These elements are highlighted as crucial to guaranteeing compliance according to the findings of the study.
This article was included due to its evidence-based and complete perspective in identifying the fundamental information needed for the application of hand hygiene education and check programs, which in turn supports the proposed intervention.
Evidence Using the MEAL Plan Format
Main Point:
The findings of the present review attest that the establishment and enforcement of a successful hand hygiene training and audit scheme have a positive impact in raising the general levels of hand hygiene among the staff, leading to decreased HAI rates.
Evidence:
Cultivating culture through training and feedback, over and over, the literature reveals that hand hygiene compliance is improved. (McLaws, 2020) compared a range of studies and concluded that frequent training and follow-up increase the staff members’ hand hygiene compliance level and help to decrease HAIs. Approximately, Alzyood et al. (2020) pointed the indication of hand hygiene during COVID-19; the teaching and observation enhanced the practices.
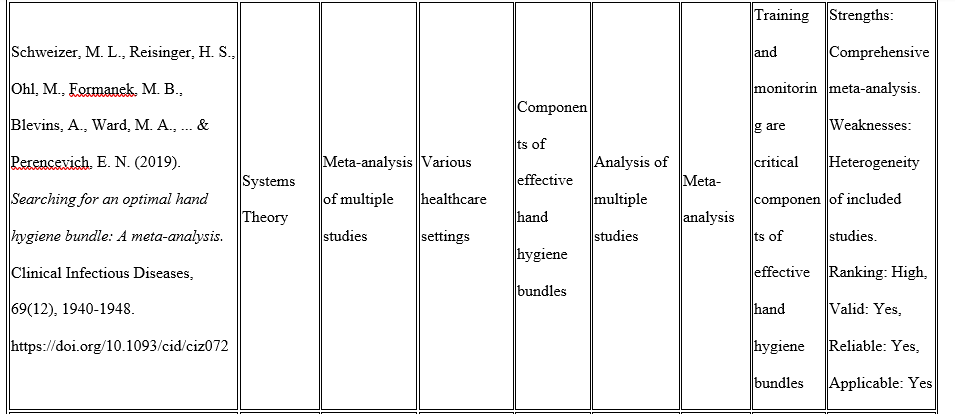
In the recent past, Boyce and Pittet (2019) highlighted guidelines that stress the importance of availing highly structured programs as well as constantly assessing skill development to promote proper hand hygiene. As discovered by Schweizer et al. (2019) in their meta-analysis of patient and staff hand hygiene, training and monitoring were deemed vital when implementing effective hand hygiene bundles.
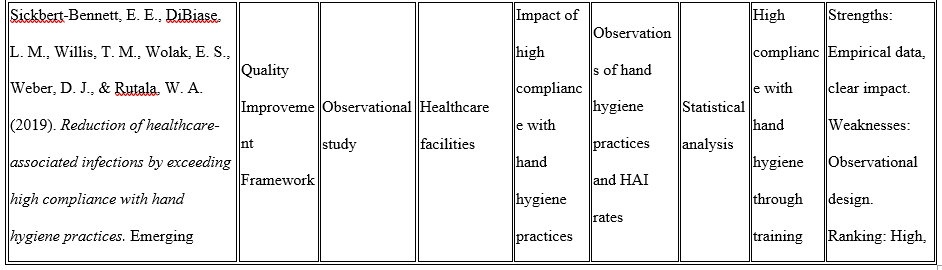
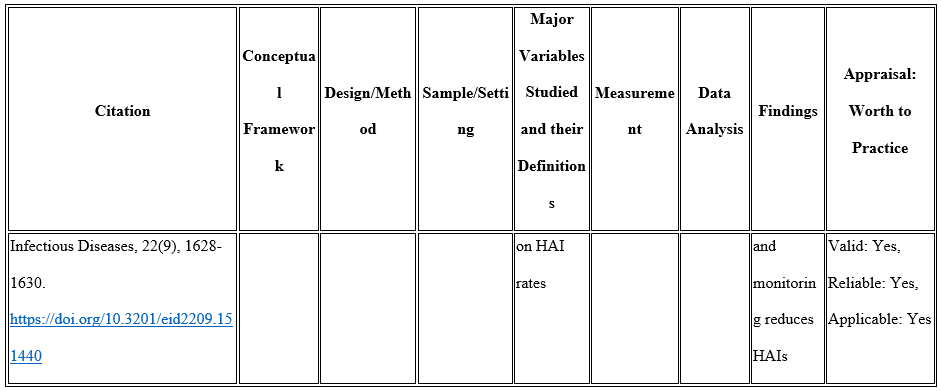
Lastly, using the cross-sectional self-administered questionnaire survey, Sickbert-Bennett et al. (2019) showed that increasing the overall compliance level through staff training and adherence monitoring will decrease HAIs’ occurrence.
Unanswered Questions
While the evidence strongly supports the proposed intervention, several unanswered questions remain that could guide further research and improve implementation: While the evidence strongly supports the proposed intervention, several unanswered questions remain that could guide further research and improve implementation:
Sustainability of Compliance:
Although several works present an increase in the hand hygiene rates shortly after interventions in various settings, the durability of such changes has not been clearly defined. Further research should be made to establish how to ensure that the levels of compliance remain high in the long run.
Cost-Effectiveness:
There is more research required to understand the economic implications of having continually train and monitor employees. More studies should be carried on cost and benefits in an aim to bring out more light on the financial implications to health organizations.
Impact on Different Healthcare Settings:
The papers reviewed in the course of this paper mainly include investigation carried out in hospital contexts. Subsequent studies should be implemented to find out the applicability of the intervention in other models of healthcare delivery units for example outpatient clinics, long-term care facilities or community health centers.
Quality of the Evidence, Including Strengths and Weaknesses
To support the notion of implementing the training and monitoring of hand hygiene, several types of studies with methodological differences were used. However, a critical appraisal of these strengths and limitations of this evidence is warranted to look at the possibilities of generalizability, and the objects for future research.
Strengths:
Diverse Methodologies:
The data sources include systematic reviews, meta-analyses, observational studies, and guideline reviews. This diversity increases the general credibility and sturdiness of the identified results (McLaws, 2020).
Consistency of Findings:
In general, the various analyses conducted in various institutions reveal a similar conclusion, which is that training and monitoring enhance the levels of hand hygiene compliance and, concurrently, decrease HAIs. This consistency contributes to the development of the credibility of the proposed intervention (Boyce & Pittet, 2019; Sickbert-Bennett et al . , 2019).
Relevance to Current Context:
Several papers describe the effects of the COVID-19 pandemic on handwashing behavior, thus, marking the work very timely and important about modern-day global health interests (Alzyood et al., 2020).
Weaknesses
Limited Long-Term Data:
Most of the research targets the issues in the short-run. Currently, there is limited evidence on whether sustained improvements within the areas of hand hygiene have been attained in the long run (McLaws, 2020; Schweizer et al. , 2019).
Context-Specific Findings:
The majority of studies are carried out in the complex environment of the hospital which might restrain the possibility of progressing the results to other types of healthcare premises including outpatient facilities or long-term care homes (Boyce & Pittet, 2019).
Potential Bias:
There can be some bias in certain types of research: observer bias in observational studies, and publication in systematic review and meta-analysis. These biases can influence the reliability of the findings according to (Sickbert-Bennett et al., 2019).
Conclusion
In conclusion, the synthesis of recent literature confirms the effectiveness of the intervention, which includes the development and subsequent training of staff accompanied by the regular monitoring of hand hygiene among HCWs. The body of literature from other studies shows that such approaches result in great improvement in universal hand washing and reduction in HAIs.
The results of numerous general interventions in terms of patients’ quality of life were sourced from systematic reviews, meta-analysis, observational studies, and guideline reviews to encourage the credibility of this intervention. Certificate Some reservations such as short-term data and sources, concern have been made but seen in a broader context, the evidence quality is good.
In the future, studies should extend their follow-up period and examine costs, other contexts besides hospitals, additional treatments in combination with the proposed intervention, patients’ perspectives, and contextual factors and organizational environments to continue improving upon the proposed intervention.
In these areas, the training and monitoring of hand hygiene in health care ought to be improved thus the following lessons can be feasible in ensuring there will be no formation of HAIs: For this reason, the outlined comprehensive approach offers a good platform for securing the stake holder’s support and subsequently implementing a hand hygiene intervention in practice. Read more about our sample NURS FPX 8045 Assessment 4 Interprofessional Communication and Practice Gap for complete information about this class.
References
Bogossian, F. E., Cant, R. P., Ballard, E. L., Cooper, S. J., Levett‐Jones, T. L., McKenna, L. G., Ng, L. C., & Seaton, P. C. (2019). Locating “gold standard” evidence for simulation as a substitute for clinical practice in prelicensure health professional education: A systematic review. Journal of Clinical Nursing, 28(21-22), 3759–3775.
https://doi.org/10.1111/jocn.14965
Edwards, A., Zweigenthal, V., & Olivier, J. (2019). Evidence map of knowledge translation strategies, outcomes, facilitators and barriers in african health systems. Health Research Policy and Systems, 17(1).
https://doi.org/10.1186/s12961-019-0419-0
Fagan, A. A., Bumbarger, B. K., Barth, R. P., Bradshaw, C. P., Cooper, B. R., Supplee, L. H., & Walker, D. K. (2019). Scaling up evidence-based interventions in US public systems to prevent behavioral health problems: Challenges and opportunities. Prevention Science, 20(8), 1147–1168.
https://doi.org/10.1007/s11121-019-01048-8
Khan, G., Kagwanja, N., Whyle, E., Gilson, L., Molyneux, S., Schaay, N., Tsofa, B., Barasa, E., & Olivier, J. (2021). Health system responsiveness: A systematic evidence mapping review of the global literature. International Journal for Equity in Health, 20(1).
https://doi.org/10.1186/s12939-021-01447-w
Lundmark, R., Hasson, H., Richter, A., Khachatryan, E., Åkesson, A., & Eriksson, L. (2021). Alignment in implementation of evidence-based interventions: A scoping review. Implementation Science, 16(1).
https://doi.org/10.1186/s13012-021-01160-w
Malterud, K. (2018). The impact of evidence-based medicine on qualitative metasynthesis: Benefits to be harvested and warnings to be given. Qualitative Health Research, 29(1), 7–17.
https://doi.org/10.1177/1049732318795864
Nadalin Penno, L., Davies, B., Graham, I. D., Backman, C., MacDonald, I., Bain, J., Johnson, A. M., Moore, J., & Squires, J. (2019). Identifying relevant concepts and factors for the sustainability of evidence-based practices within acute care contexts: A systematic review and theory analysis of selected sustainability frameworks. Implementation Science, 14(1).
https://doi.org/10.1186/s13012-019-0952-9
Ryder, M., Jacob, E., & Hendricks, J. (2020). An integrative review to identify evidence of nurse practitioner‐led changes to health‐care delivery and the outcomes of such changes. International Journal of Nursing Practice, 26(6).
