- NURS FPX 6610 Assessment 2 Patient Care Plan.
NURS FPX 6610 Assessment 2 Patient Care Plan
Explore our assessment NURS FPX 6610 Assessment 1 for more information.
Reference
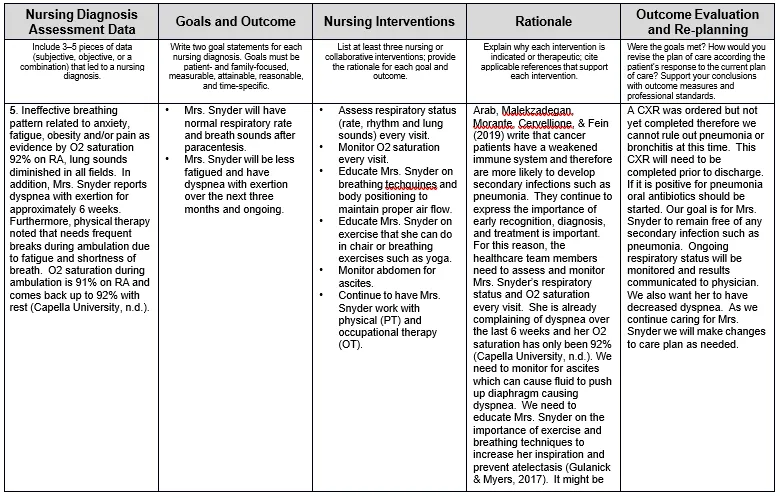
Arab, T., Malekzadegan, M. R., Morante, J., Cervellione, K. L., & Fein, A. M. (2019). Nonresolving pneumonia in the setting of malignancy.
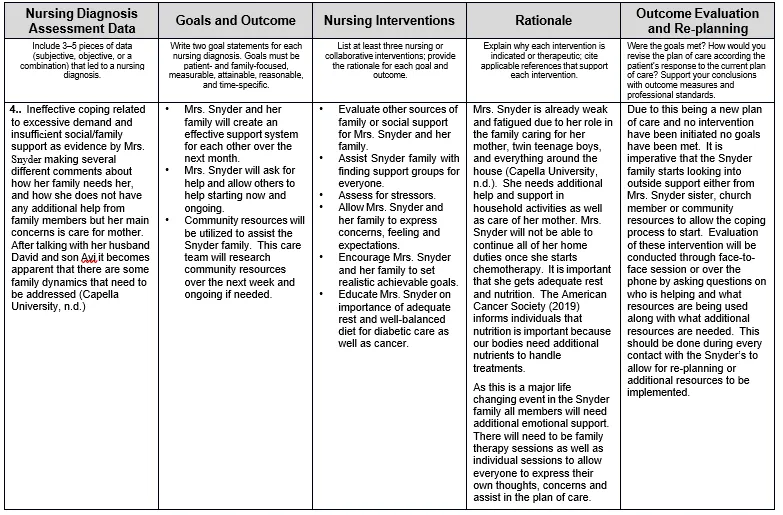
Current Opinion in Pulmonary Medicine. 25(4), 331-335. doi: 10.1097/MCP.0000000000000588 American Cancer Society. (2019). Benefits of good nutrition during cancer treatment. Retrieved from
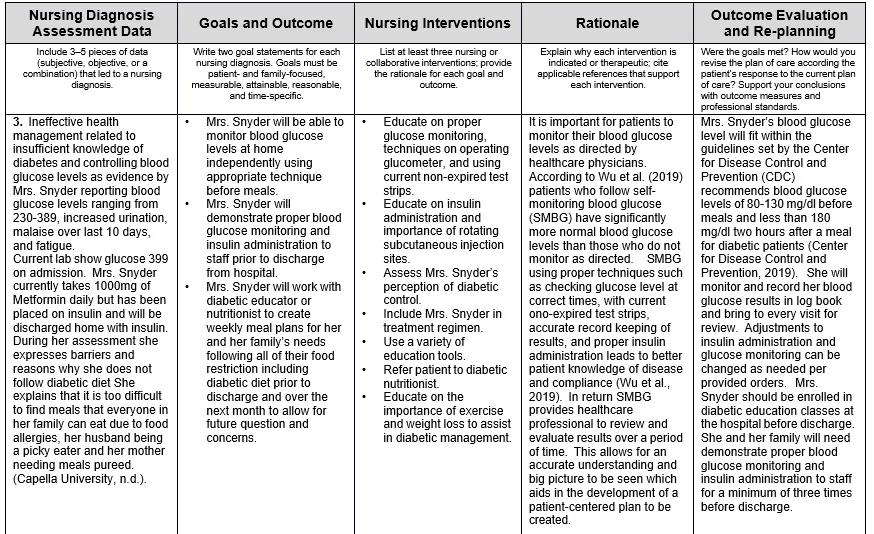
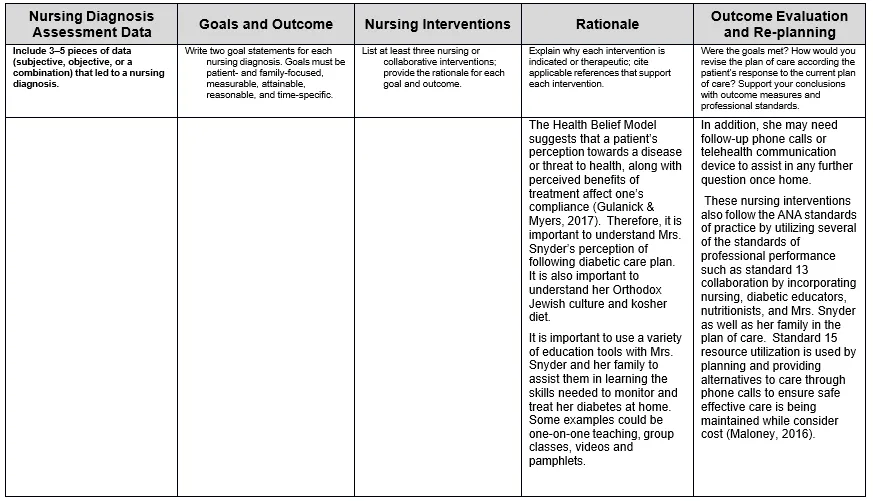
Center for Disease Control and Prevention. (2019). Manage Blood Sugar. Retrieved from https://www.cdc.gov/diabetes/managing/manage-blood-sugar.html.
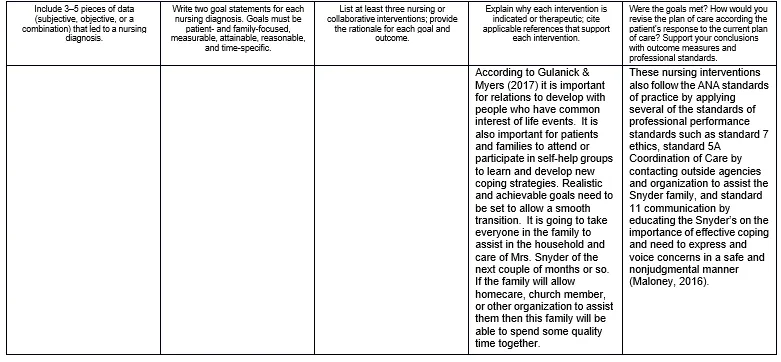
Gulanick, M., & Myers, J. L. (2017). Nursing Care Plans (9th ed.). St. Louis, MO: Elsevier.
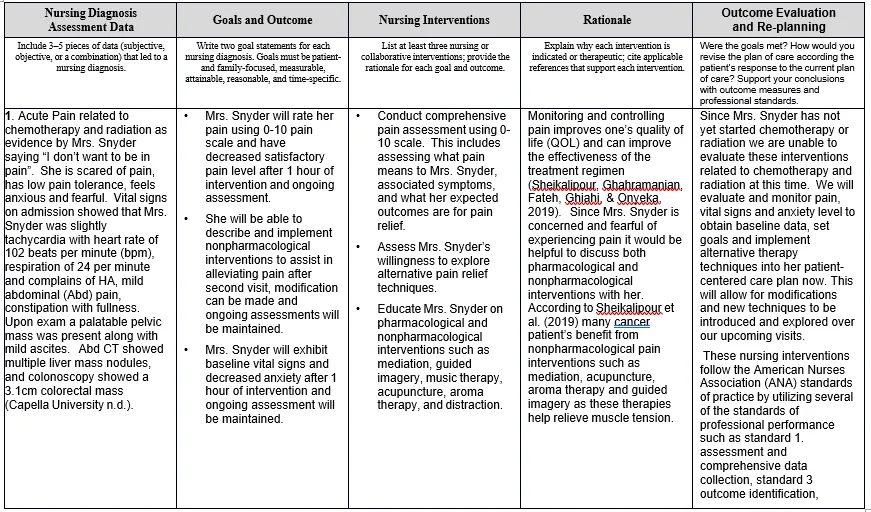
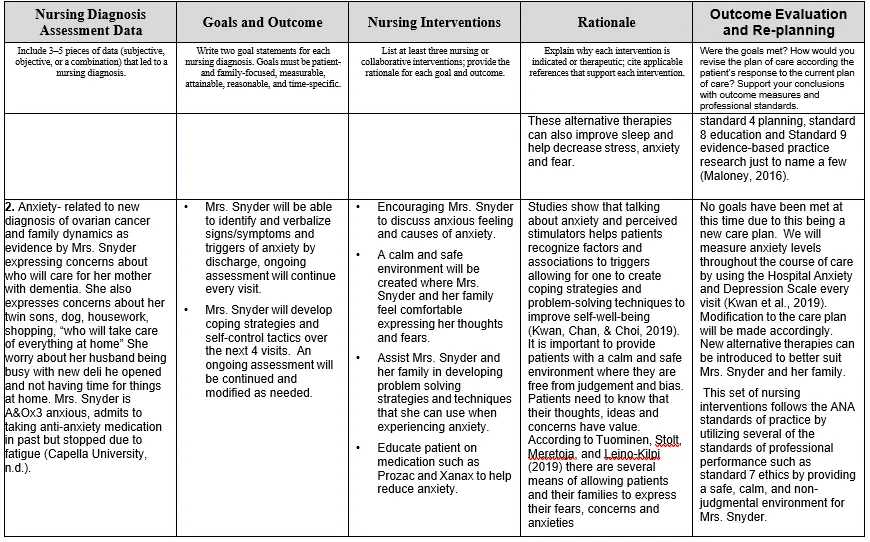
Kwan, C. W., Chan, C. W., & Choi, K. C. (2019). The effectiveness of a nurse-led short-term life review intervention in enhancing the spiritual and psychological well-being of people receiving palliative care: A mixed method study. International Journal of Nursing Studies, 91, 134–143. doi: 10.1016/j.ijnurstu.2018.12.007
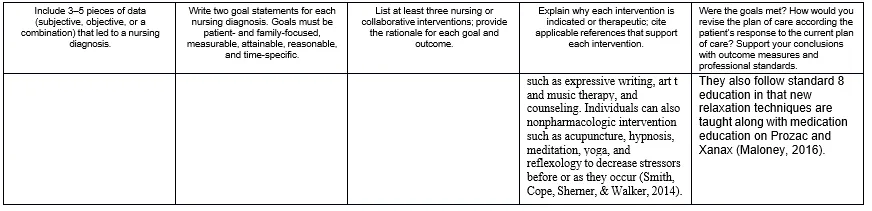
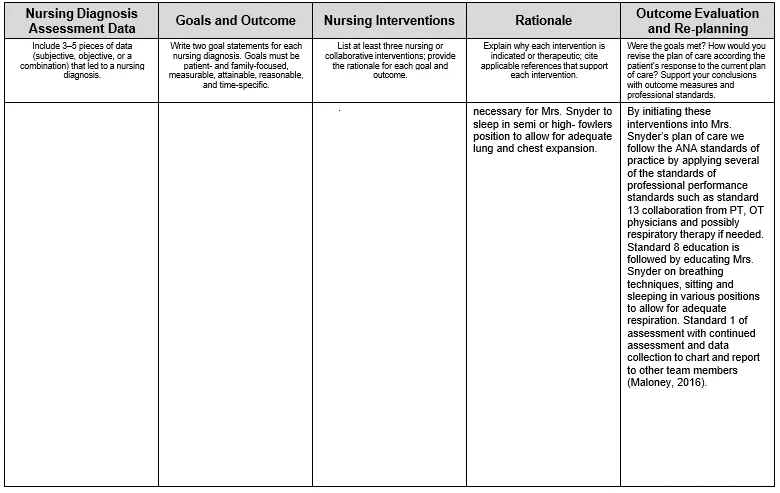
Maloney, P. (2016). Nursing professional development: Standards of professional practice. Journal for Nurses in Professional Development.
32(6), 327-330. doi: 10.1097/NND.0000000000000300
Sheikhalipour, Z., Ghahramanian, A., Fateh, A., Ghiahi, R., & Onyeka, T. C. (2019). Quality of life in women with cancer and its influencing factors. Journal of Caring Sciences, 8(1), 9-15. doi:http://dx.doi.org.library.capella.edu/10.15171/jcs.2019.002
Smith, P.R., Cope, D., Sherner, T. L., & Walker, D.K. (2014). Update on research-based interventions for anxiety in patients with cancer.
Clinical Journal of Oncology Nursing. 18(6), 5-16. doi: 10.1188/14.CIONS3.5-16
Tuominen, L., Stolt, M., Meretoja, R., & Leino-Kilpi, H. (2019). Effectiveness of nursing interventions among patients with cancer: An overview of systematic reviews. Journal of Clinical Nursing, 28(13-14), 2401–2419. doi: 10.1111/jocn.14762
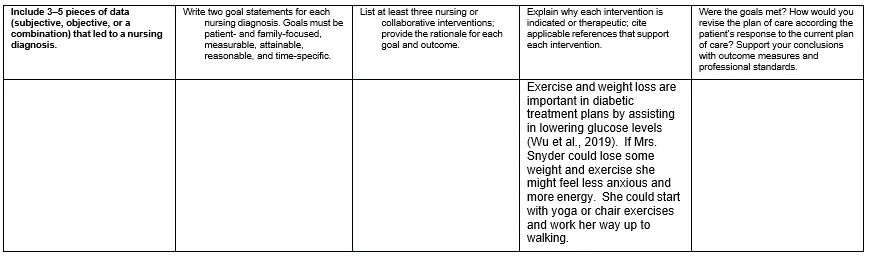
Wu, J., Su, X., Lian, H., Lin, A., Wei, H., & Hu, J. (2019). Quality control circle improves self-monitoring of blood glucose in type 2 diabetic patients. Australian Journal of Advanced Nursing (Online), 36(3), 22-28. Retrieved from
