- NURS FPX 9904 Assessment 1 CBT Sessions and Motivational Intervening
Project Summary Report
From the study, it is evident that the worldwide epidemic of opioids has been ranked as one of the most pressing challenges in public health in the present generation. This proposal aimed at implementing possible improvements in the treatment plans for clients with opioid use disorder who could benefit from CBT and MI. This enables individuals to indulge in substance abuse, which is forcing an abnormal increase in the rates of illness and mortality as well as being the number one drain on the economies of the countries.
The qualitative inquiry thus aimed at evaluating the efficacy of the two multifaceted therapeutic modalities of treatment in reducing the readmission rates and enhancing the adherence of the patients afflicted with opioid dependency. It was the goal of the project to increase the treatment efficacies of patients upon the enhancement of the conventional focus on disease pathology and psychological and physiological aspects of addicted behaviors.
The assessment report featured a project description, data gathered from several sources, an analysis of the results, and a conclusion with recommendations for further application of the interventions in many healthcare facilities. Explore our assessment DNP FPX 9904 Assessment 6 Reflection for more information.
Background and Organization Gap Analysis
According to Dydyk et al. (2024), opioid dependence disorder is a significant health issue that is present all across the world and is observed in over 16 million individuals, thus having a massive impact on the society and the economy of the countries affected by this issue. Psycho-social intervention, drug counseling, and other forms of psychological treatments and pharmacological treatments are some of the conventional treatments for drug dependence and chronic pain.
They do not, however, often fulfill the comprehensive requirements of these patients. The types of treatment that have been proven effective include Cognitive Behavioral Therapy (CBT) and Motivational Interviewing (MI). These are useful for the head and, occasionally, the body involved in the creation of addiction. The challenge arises from placing the ideas systematically and sequentially into a whole treatment process.
Since the beginning of the graduate project, the project site relied on standard intervention methods such as medication, therapy, and counseling. The methods failed to pay adequate attention to every addict’s circumstances as needed by designing treatments best for each of them (Volkow & Blanco, 202). There were high readmission rates, and even though they needed ongoing care, patients improved slower than before. The currently used methods did not address dependency’s root psychological features so that they may be better.
NURS FPX 9904 Assessment 1 CBT Sessions and Motivational Intervening
The first important issue we identified in the treatment plan approach for the project site was that it failed to incorporate a tailored approach that integrates CBT and MI for opioid-dependent patients as part of the patient-centered, interdisciplinary model for patients in primary care settings. The current rules were insufficient for achieving the needed outcomes like reducing readmission rates or patient compliance with treatment regimens (S. D., Personal Communication, November 29, 2023).
Improving Addiction Treatment Efficacy
According to the utilization patterns of hospitals in the third quarter of 2023, readmissions that occur from a relapse of opioid use disorder account for half of all readmission occurrences. This indicates that what is currently being done in trying to ‘treat’ persons with drug use disorders is no longer effective (S. D, Personal Communication, November 29, 2023). Identifying this lacuna, the project site envisaged the potential of offering a patient-centered approach to the CBT plus MI regime where it would be possible to enhance the synergy of both methods. This would help reduce and close the gap and offer a more holistic understanding of addiction treatment.
This was the project’s rationale because it aimed to enhance patient results and reduce pressures on healthcare systems by assessing the efficacy of the treatments. The plan intended to exclude a “blanket approach,” where doctors lack the discretion to adapt interventions to focus on the individual risk factors, drug usage, and mental health states of the client (Pollok et al., 2019). The objectives of the undertaking were to raise efficacy and quality of care in the unit to enhance patients’ outcomes and reduce the rate of readmissions due to relapses in OUD, hence making addiction treatment more effective and compassionate.
Significance of the Practice Problem
Opioid abuse remains a significant issue, which impacts millions of people globally and considerably shatters hundreds of millions in terms of costs, lives lost, and health deterioration. The annual death figure due to drug abuse is more than seventy thousand in the USA, which underlines the significance of having efficient intervention strategies (Dydyk et al., 202 ).
The CDC and SAMHSA, along with other organizations, emphasize the concept of treatment approaches that are evidence-based and require addressing the biological, psychological, and social components of Substance Use Disorders. The project’s goal was to answer the TWICE question below: Consequently, is the number and commitment to complete treatment and/or number of readmissions within 12 weeks affected when using individualized CBT and MI (I) rather than standard treatment methods (C) to treat opioid dependents (P)?
Enhancing Opioid Treatment Through CBT and MI Integration
Coordinating between CBT and MI serves the national purpose of enhancing the quality of life for patients who are addicted to opioids (Chand et al., 202^). Generally, effective treatment for drug addicts is beneficial to the drug user and their family. It elevates well-being, reduces mortality, and enhances life in every way possible. In the health system, reasonable measures can minimize return rates, cut the amount of money spent on healthcare services, and relieve pressures on emergency services and healthcare personnel (Volkow & Blanco, 2023). Employer costs include costs of health care, medications, missed days at work due to opioid use, and crime-related expenses.
Integration of the samples followed CBT and MI to reduce readmissions and, thus, spread them out and make the situation better in the end (Pranckeviciene et al., 2022). When it comes to the issue of drug addiction, people should consider several critical cultural and moral factors, like the embarrassment of being forced to join a drug rehab program, patient privacy, and legal constraints in the management of this. sharedInstance Delivering individualized CBT and MI also respects patients’ autonomy and cultural preferences in practicing patient-centered care. This is as per the principles of ethics and generally makes the treatment much more efficient (Corbett et al., 2023).
Summary of the Evidence
Focusing on the PICOT question around the identified population of nurses catering to individuals with opioid addiction, thirty sources were regarded concerning relevancy, adherence to research methodologies, and utility in the context of the quality improvement project. The new search searched for every similar source with higher sensibility, such as CINAHL, PubMed, and the Cochrane Library. According to the findings of the current review of customized CBT and MI treatments for opioid-dependent patients, the following six main concerns can be underlined.
CBT and MI for Opioid Use Disorder Treatment and Feasibility
First of all, the obtained outcome identified that CBT can be a practical approach to treat OUD as well as chronic pain. For instance, a systematic review was carried out to determine the mental health workers’ perception of the effectiveness of CBT in the treatment of OUD conducted in Lent et al. (2021). Moreover, motivational interviewing (MI) could also be employed for the manipulative use of opioids and other drug issues; Smedslund, Stileg, and Middelthon (2011) argued that it indeed works for substance use outcomes. The project has also sought to determine whether it is feasible and how much it would be for patients to receive MI or CBT for drug use disorder and chronic pain. This is evidenced by Olmstead and colleagues’ quantitative work on the feasibility and efficacy of MI intervention methods.
In a particular group of individuals with both OUD and other mental health disorders, two treatments that have been considered are CBT and MI. One of these is MI-CARE, which was conducted by DeBar et al. Unfortunately, the conversation that has revealed the efficacy of the CBT and MI treatments indicates that there is still some critical work to be done — ensuring that these treatments are effective for people of all cultures and can be applied to them.
In a study by Adams et al. (2023), MI was noted to have good results for the increased drug users, and thus, it can be adopted in low-income settings. The topics assist us in defining what is currently known about the effectiveness and feasibility of integrating the elements of personalized CBT and MI care for opioid-dependent patients into practice for patients with OUD, the cost of the intervention, and its potential applicability to culturally diverse populations.
Quality Improvement Framework
Based on the notion that the care experience should be more logical and technical to achieve the intended goals of the doctoral project, the Plan-Do-Study-Act model was adopted as the QI framework for the project (Triplett et al., 2022). The PDSA model consists of an ongoing confirmation undertaking: repeatedly plan, do, study, and act.
When particular challenges were essential and complex, for example, when the hospital was targetting a low readmission rate among opioid-dependent patients, the reasoning process would be utilized. Stakeholder involvement and interim review were reported as highly critical in the project to meet its overall goals and objectives and all the relevant change perspectives it planned to implement (Benetato et al., 2020).
Strategic Implementation and Evaluation of Nursing Interventions
Since every project requires a comprehensive strategy for its implementation, creating a sound plan was the initial step to ensure that the QI/PI project flowed smoothly. When planning the actions of the nursing intervention, the nurses were very precise to ensure that everyone complied with all the steps and rules during the planning process. In the first step, a detailed examination and dialogue about essential practices and the ratification of the comprehensiveness of healthcare quality improvement processes were conducted by Abuzied et al. (2023). Thus, ensuring the framework’s construction helped the nurses make it possible to implement the project and proceed to the further stages effectively.
In the second stage, at the same location, nurses whose patients had assisted in overcoming drug abuse also adopted the program at the workplace. Utilizing the program in real life meant incorporating it into the working experience and introducing countless modifications to follow new regulations. During the third strategy cycle, the nurses endeavored to ascertain the effectiveness of the developed strategy.
In collecting data, they incorporated motivated interviews and cognitive behavioral therapy to gather both qualitative and quantitative data. The final aspect of successful treatment utilization was to tailor the current methods to clients’ conditions. This ensured that each patient received individual attention, coordination, and documented care to enhance their outcome. Which, as Wasim et al. (2023) called it, not only improved the outcomes of the treatments but also built a healthcare environment that was beneficial and patient-focused.
NURS FPX 9904 Assessment 1 CBT Sessions and Motivational Intervening
One of the significant focuses within a portion of the project was to collect and evaluate data, which ensured that a particular action and work implemented within the project met its purpose (Serwer, 2021). As Blanchard et al. (2019) pointed out, implementing an EHR in the healthcare delivery system ensures that the collected, verified, and normalized data is done correctly.
This makes it possible to have quality and sound research [1]. Also, simple quantitative aspects were examined in the study; therefore, it was easy to disseminate basic quantitative details such as the rate of return, increased applications for CBT treatments, and even patients’ compliance with the treatment regimens.
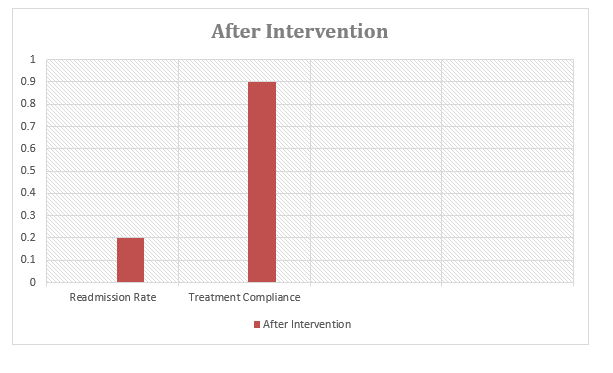
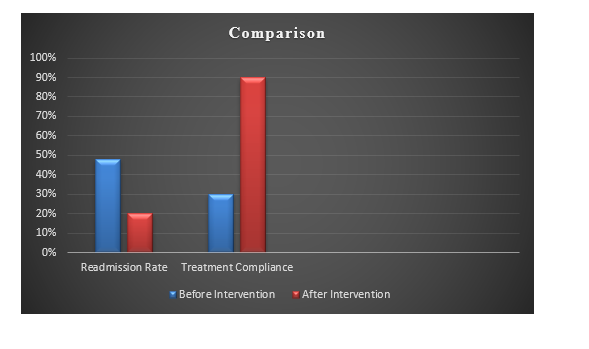
Regarding objectives, the project has the following: to reduce drug addicts’ readmission rate (Kelley et al., 2022). CBT lessons and contingency management can be combined to provide more effective treatment. According to the duration and type of work, the expected objectives include research on the way to reduce the readmission rate to an average of 20%, eliminating the possibility of 10% of patients’ noncompletion of CBT, establishing an average of not less than 90% completion within 12 weeks (Barry et al., 2020).
Even though an organization may have to deal with staff reluctance and cultural incompetence, and even though one can usually identify factors and support that connect to the goal of a project, the next question to address is how to better understand those factors and support.
Project Description
It was planned and implemented in various healthcare facilities, from hospitals to basic care centers and specialized treatment programs. I observed that numerous tools were available to perform the treatments and assess the results, and the patients had different backgrounds. In regards to the population, only outpatients with OUD and those over the age of 18 who were motivated to attend specialized CBT and MI group classes had the chance to participate in the project.
Patient-Centered Education and Intervention Strategies
The latter was excluded due to medical conditions such as severe mental disorders and inability to speak English; the patient did not choose to use a translator since language services were not provided, and those in another treatment program conflicted with this one. The project also ensured it had a defined and valuable group of employees to work with while avoiding the confusion of including various employees who could not be helpful to the project while still staying within the healthcare medium.
Education in the form of individualized CBT and MI lessons was employed in the intervention. Each specifically offered coverage for both the psychological and physical aspects of substance misuse. Methods including cognitive restructuring, controlled problem-solving, and stress-coping skills (Chand et al., 2023) in CBT sessions assisted patients with substance dependence in identifying and modifying their distressed thinking patterns and activities.
In MI meetings, the focus was to enhance the individual patient’s intrinsic motivation for change, coming up with the states or reasons why the change was not desirable. The meetings were held based on the strategies and values that focus on the client, empathy, teamwork, and support (Fragkiadaki et al., 2023).
Project Evaluation Results
Using instruments such as the ORT and only admitting the practices that fall under AQR Qualitative analysis guaranteed the outcomes were accurate. It is worth adding that best practices were implemented to collect the data and make initial evaluations constantly; therefore, the project’s results improved even more. This laid the foundation for further examination and use across various healthcare environments.
Given that unique CBT and MI tools were used, this study applied a mixed-methods approach to understand how well it supported those with Opioid Use Disorder (OUD). Again, the data collection involved quantitative and qualitative methods to ensure an optimal understanding of the treatments applied.
According to guidelines adopted in most healthcare research, quantitative data and subjects’ feelings were collected using the mixed research method. The Institutional Review Board (IRB) approved all the methods through which the data was collected to ensure they were viable and safeguarded the participants’ welfare.
Actual quantitative data were collected utilizing global outcome measures that must have been established. For these, they considered factors such as return rates and compliance with treatment regimens. Only appraisal icons, such as figures, were applied to assess the outcome (Cooksey, 2020).
Data Collection Methods and Analysis
The drug Risk Tool (ORT) was the primary method to measure numeric data. The following specifics were noted regarding the data collection methods used: Dependability has gotten 0. 83 and has been validated in the previous research as a tool capable of correctly estimating the rate of drug abuse (Brott et al., 2022). ORT authors were allowed to use their abbreviations, which provided that no violations of the rights to an intellectual product would be made. With the help of the tool, it became possible to employ the same metric to measure the risk factors within patients and their impact, making it easier to compare the effectiveness of interventions.
On the other hand, qualitative information was obtained through structured interviews with the patients, the healthcare providers, and every project stakeholder involved. Fragkiadaki et al. (2023) conducted a qualitative study to explore participants’ emotional experiences, perceptions, and views about CBT and MI treatment. They were designed to reveal how satisfied the subjects were with the treatments and how they believed they impacted the physical health and well-being of the patients.
These interviews collected qualitative data that were analyzed using thematic analysis and had similar themes and trends to give additional information on how well the researched intervention has worked. It made the researchers gain insights about issues concerning the subjects where the study was done, besides knowing the outside influences on the outcome of the interjection.
NURS FPX 9904 Assessment 1 CBT Sessions and Motivational Intervening
The formal assessment was conducted continuously during the project alongside daily discussions with stakeholders to check how the treatments were being performed (Corbett et al., 2023). The nature of the intervention meant that the methods could be modified during the implementation process to address new emergent issues and improve the process and the sustainability of the intervention. Face-to-face contact with patients, doctors, and managers regularly provided helpful knowledge about the benefits and drawbacks of the treatments to make them continue enhancing the treatments to meet their needs regularly.
Based on various suggestions by Nair (2023), the project incorporated end-result sorting, matching, and multivariable regression modeling as part of its analysis approach to address possible influence factors. The study used sensitivity analysis to test all possible influences that might have distorted the data to guarantee that the correct results were determined. The discussed methods may enhance the relevancy of the project’s findings for other settings. They can thus contribute to the utilization of evidence-based practice in drug abuse treatment, particularly through NURS FPX 9904 Assessment 1 CBT Sessions and Motivational Intervening, which is a key approach in addressing patient needs effectively.
Effectiveness of CBT and MI
Specific details of the treatments implemented are Cognitive Behavioural Therapy (CBT) and Motivational Interviewing (MI), and the following statistical tests were conducted to compare the efficiency of the treatments. In doing so, the following conclusions should be made for the unequal variances t-test: Descriptive statistics, including the t-test, means, and standard deviations, were applied. Anovas were used with individual t-tests to compare the return rates and the treatment compliance before and after the intervention. Notably, thematic analysis was employed to identify themes and ideas equivalent to the provider and patient comments.
The one thing that was monitored was the number of opioid-dependent patients who would be admitted to the hospital after the intervention. Their data analysis indicated that the number of readmissions was reduced more than in the case of attempting other individual CBT and MI approaches. Pre-intervention, 48% of the patients they observed had at least one readmission. This reduced to 20% (p < 0.05, S.D.). During the post-intervention assessment, only 20 percent of the participants reported that they had experienced this feeling (Personal Communication, 2023). The drastic reduction in readmission for the targeted samples indicates that the treatments reduced the probability of readmission among patients with HF, showcasing the effectiveness of NURS FPX 9904 Assessment 1 CBT Sessions and Motivational Intervening in improving patient outcomes.
Figure 1
Before Intervention Rate of Readmission and Treatment Compliance
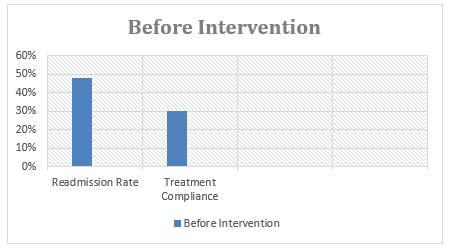
Figure 2
After Intervention Rate of Readmission and Treatment Compliance
References
Abuzied, Y., Alshammary, S. A., Alhalahlah, T., & Somduth, S. (2023). Using FOCUS-PDSA quality improvement methodology model in healthcare: Process and outcomes. Global Journal on Quality and Safety in Healthcare, 6(2). https://doi.org/10.36401/jqsh-22-19
Adams, A., Williams, T., Stein, D. J., Goodman Sibeko, S., S., & Rollnick, S. (2023). Motivational interviewing interventions for harmful substance use amongst adults in low- and middle-income countries (LMICS): A systematic review. MedRxiv (Cold Spring Harbor Laboratory). https://doi.org/10.1101/2023.09.15.23295607
Amin, M., Reza Davasaz Irani, Fattahi, P., & Sirus Pakseresht. (2023). Effects of brief cognitive behavioral therapy on mental health in substance-related disorder: A randomized controlled trial. BMC Psychiatry, 23(1). https://doi.org/10.1186/s12888-023-05413-4
Barry, D. T., Beitel, M., Cutter, C. J., Fiellin, D. A., Kerns, R. D., Moore, B. A., Oberleitner, L., Madden, L. M., Liong, C., Ginn, J., & Schottenfeld, R. S. (2019). An evaluation of the feasibility, acceptability, and preliminary efficacy of cognitive-behavioral therapy for opioid use disorder and chronic pain. Drug and Alcohol Dependence, 194, 460–467. https://doi.org/10.1016/j.drugalcdep.2018.10.015
Benetato, B. B., Tillman, J., Corbett, R. W., & Hodges, A. (2020). The Doctor of Nursing Practice project data collection tool. Nursing Education Perspectives, 42(6), 72–73. https://doi.org/10.1097/01.nep.0000000000000643
Blanchard, J., Weiss, A. J., Barrett, M. L., Stocks, C., Owens, P. L., Coffey, R., & Heslin, K. C. (2019). Readmissions following inpatient treatment for opioid-related conditions. Substance Use & Misuse, 54(3), 473–481. https://doi.org/10.1080/10826084.2018.1517174
Brott, N. R., Peterson, E., & Cascella, M. (2022). Opioid risk tool. Nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK553147/
Buckner, J. D., Scherzer, C. R., Crapanzano, K. A., & Morris, P. E. (2023). Group cognitive behavioral therapy for substance use disorders among psychiatric inpatients in a medically underserved area: An intervention for opioid misuse. Public Health Reports, 138(1_suppl), 90S95S. https://doi.org/10.1177/00333549231170219
Buckner, J. D., Walukevich-Dienst, K., Crapanzano, K. A., Tucker, R. P., & Tynes, L. L. (2021). Brief motivational interviewing–based interventions for opioid misuse in hospital settings. Translational Issues in Psychological Science, 7(2), 114–129. https://doi.org/10.1037/tps0000280
CDC. (2022). Motivational interviewing to help your patients seek treatment: Opioids. Cdc.gov. https://www.cdc.gov/opioids/addiction-medicine/conversation-starters/motivational-interviewing.html
Chand, S. P., Kuckel, D. P., & Huecker, M. R. (2023). Cognitive behavior therapy (CBT). Nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK470241/
Cooksey, R. W. (2020). Descriptive statistics for summarising data. Illustrating Statistical Procedures: Finding Meaning in Quantitative Data, 15, 61–139. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7221239/
Corbett, A. P., Parke, S., Bear, H. A., & Clarke, T. (2023). Barriers and facilitators to implementing evidence‐based interventions in children and young people’s mental health care – a systematic review. Child and Adolescent Mental Health. https://doi.org/10.1111/camh.12672
DeBar, L. L., Bushey, M. A., Kroenke, K., Bobb, J. F., Schoenbaum, M., Thompson, E. E., Justice, M., Zatzick, D., Hamilton, L. K., McMullen, C. K., Hallgren, K. A., Benes, L. L., Forman, D. P., Caldeiro, R. M., Brown, R. P., Campbell, N. L., Anderson, M. L., Son, S., Haggstrom, D. A., & Whiteside, L. (2023). A patient-centered nurse-supported primary care-based collaborative care program to treat opioid use disorder and depression: Design and protocol for the MI-CARE randomized controlled trial. Contemporary Clinical Trials, 107124. https://doi.org/10.1016/j.cct.2023.107124
DeBar, L., Mayhew, M., Benes, L., Bonifay, A., Deyo, R. A., Elder, C. R., Keefe, F. J., Leo, M. C., McMullen, C., Owen-Smith, A., Smith, D. H., Trinacty, C. M., & Vollmer, W. M. (2021). A primary care-based cognitive behavioral therapy intervention for long-term opioid users with chronic pain. Annals of Internal Medicine, 175(1). https://doi.org/10.7326/m21-1436
Dydyk, A. M., Jain, N. K., & Gupta, M. (2024). Opioid Use Disorder. Nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK553166/#:~:text=%5B1%5D%20OUD%20affects%20over%2016
Fragkiadaki, E., Cotterill, N., Rice, C., Smith, J. A., & Nizza, I. E. (2023). Evaluating the feasibility and acceptability of an integrative group psychological intervention for people with Multiple Sclerosis: A study protocol. Public Library of Science One, 18(7), https://doi.org/10.1371/journal.pone.0288295
Johnson, A. E., Routh, S., Taylor, C., Leopold, M., Beatty, K., McNamara, D., & Davis, E. (2021). Developing and implementing a mobile health heart failure self-care program to reduce readmissions: A patient-centered outcomes research randomized controlled trial (Preprint). JMIR Cardio, 6(1). https://doi.org/10.2196/33286
Jordan, J., Clarke, S. O., & Coates, W. C. (2021). A practical guide for conducting qualitative research in medical education: Part 1—How to interview. Academic Emergency Medicine Education and Training, 5(3). https://doi.org/10.1002/aet2.10646
Kelley, A. T., Incze, M. A., Baylis, J. D., Calder, S. G., Weiner, S. J., Zickmund, S. L., Jones, A. L., Vanneman, M. E., Conroy, M. B., Gordon, A. J., & Bridges, J. F. P. (2022). Patient-centered quality measurement for opioid use disorder: Development of a taxonomy to address gaps in research and practice. Substance Abuse, 43(1), 1286–1299. https://doi.org/10.1080/08897077.2022.2095082
Kumar, A., Seewal, R., Jain, D., & Kaur, R. (2024). Framework for personalized chronic pain management: harnessing AI and personality insights for adequate care. Journal of Artificial Intelligence and Technology, 51(21). https://doi.org/10.37965/jait.2024.0457
Lent, M. R., Callahan, H. R., Womer, P., Mullen, P. M., Shook, C. B., DiTomasso, R. A., Felgoise, S. H., & Festinger, D. S. (2021). A mental health professional survey of cognitive‐behavioral therapy for the treatment of opioid use disorder. Journal of Clinical Psychology, 77(7), 1607–1613. https://doi.org/10.1002/jclp.23170
Nair, A. (2023). Confounding Variables | Definition, Examples & Controls. Enago.com https://www.enago.com/academy/confounding-variables/#:~:text=Confounding%20variables%2C%20also%20referred%20to
Olmstead, T. A., Yonkers, K. A., Forray, A., Zimbrean, P., Gilstad-Hayden, K., & Martino, S. (2020). Cost and cost-effectiveness of three strategies for implementing motivational interviewing for substance misuse on medical inpatient units. Drug and Alcohol Dependence, 214, 108156. https://doi.org/10.1016/j.drugalcdep.2020.108156
Pollok, J., E.M J., Carson, K., Esterman, A., S., B. J., & Júlio Licinio. (2019). Psychological therapies for the treatment of depression in chronic obstructive pulmonary disease. The Cochrane Library, 2019(4). https://doi.org/10.1002/14651858.cd012347.pub2
Pranckeviciene, A., Saudargiene, A., Stonciene, J. G., Liaugaudaite, V., Bulanova, I. G., Simkute, D., Naginiene, R., Dainauskas, L. L., Ceidaite, G., & Burkauskas, J. (2022). Validation of the patient health questionnaire-9 and the generalized anxiety disorder-7 in the Lithuanian student sample. Public Library of Science One, 17(1), https://doi.org/10.1371/journal.pone.0263027
Serwer, G. A. (2021). Data management and integration with electronic health record systems. Cardiac Electrophysiology Clinics, 13(3), 473–481. https://doi.org/10.1016/j.ccep.2021.05.001
Smedslund, G., Berg, R. C., Hammerstrøm, K. T., Steiro, A., Leiknes, K. A., Dahl, H. M., & Karlsen, K. (2011). Motivational interviewing for substance abuse. Campbell Systematic Reviews, 7(1), 1–126. https://doi.org/10.4073/csr.2011.6
Triplett, N. S., Woodard, G. S., Johnson, C., Nguyen, J. K., AlRasheed, R., Song, F., Stoddard, S., Mugisha, J. C., Sievert, K., & Dorsey, S. (2022). Stakeholder engagement to inform evidence-based treatment implementation for children’s mental health: A scoping review. Implementation Science Communications, 3(1). https://doi.org/10.1186/s43058-022-00327-w
Volkow, N. D., & Blanco, C. (2023). Substance use disorders: A comprehensive update of classification, epidemiology, neurobiology, clinical aspects, treatment and prevention. World Psychiatry, 22(2), 203–229. https://doi.org/10.1002/wps.21073
Wasim, A., Sajan, M., & Majid, U. (2023). Patient-centered care frameworks, models and approaches: An environmental scan. Patient Experience Journal, 10(2), 14–22. https://doi.org/10.35680/2372-0247.1806
