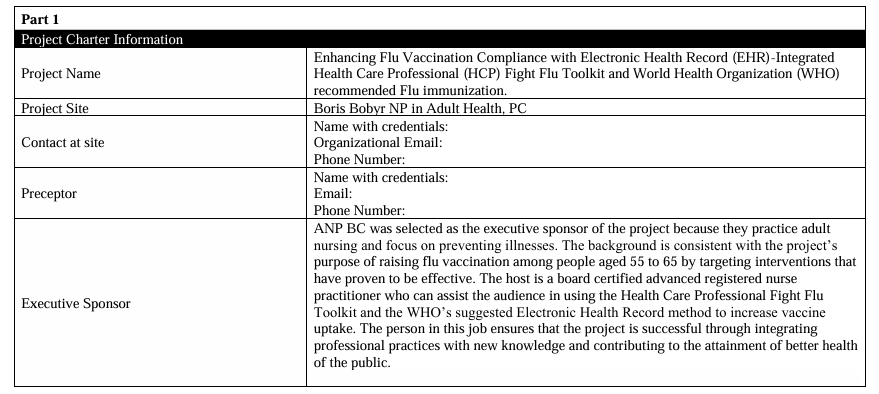
NURS FPX 9100 Assessment 6
Project Charter
After reviewing the detailed assignment instructions in the course for each of the Project Charter components, use this template to complete your project charter, replacing the instructional text in the cells with the required information.
PLEASE NOTE. THIS PROJECT:
- It cannot be implemented and measured until after you have IRB approval from Capella and your site if indicated. The gap analysis for the Project Charter is a retrospective data analysis.
- So, you cannot make your whole project a retrospective data analysis, as it is just a small part of planning the project.
- Sections need to be written in a narrative with grammatically correct sentences unless indicated in the specific section.
Are you Looking for guidance for NURS FPX 9100 Assessment 6? Our experts are here to assist you. Reach out to us for support today.
SWOT Analysis and Business for Project
Strengths
Some of the organization’s assets that can support the project include a strong leadership team, availability of resources like the HCP Fight Flu Toolkit which is evidence informed and the use of an Electronic Health Record system.
The group is also concerned with prevention of diseases and seeking for new solutions to problems, which is in consonance with the project objectives. Proper tools for a smooth adoption process include money for staff training and money for upgrading the EHR-system.
Weaknesses
Some barriers that may hinder the success of the project include: Health care personnel or patients’ resistance, inadequate staff or facilities, and challenges in integrating the HCP Fight Flu Toolkit with the current EHR system.
There could also be challenges that are as a result of unsuccessful efforts of undertaking similar projects in the past or people who are involved in the project do not support it. The solution may also have less of an effect if there are cultural or language barriers in the target group (Schouten et al. , 2020).
Opportunities
The project allows the group to demonstrate that it is concerned with the quality growth and the use of proven strategies. Pyne et al. (2023) argue that if the organization is able to effectively implement the HCP Fight Flu Toolkit and EHR integration it will be hailed as the leader preventive health care and enhance its reputation in the society.
NURS FPX 9100 Assessment 6 Project Charter
It may help to increase the vaccination of people and reduce the cost of health care and therefore get more funds or agreements. The project provided knowledge that can be applied in the future in an attempt to enhance the patient outcomes or tackle other health related issues.
Threats
Some other factors that are out of the control of the implementers of the project could include changes in rules and regulations of healthcare, payment policies, or perception of the community on vaccinations among other things could make the project to fail.
One more threat could be posed by other healthcare workers who present the same kind of programmes or alternative ways of increasing vaccination coverage (Kopsidas et al. , 2020). Such events as a disease outbreak or natural disasters could hinder the project implementation or alter the organizational goals, which would slow down the project.
References
Bach, A. T., Kang, A. Y., Lewis, J., Xavioer, S., Portillo, 1., & Goad, J. A. (2019). Addressing common barriers in adult immunizations: A review of interventions. Nryrrr dr r irn r›/ Vo‹ ‹ inrs, /8(1 l ), l l 67— 1 1 85.
https://doi.ore/1O.1OhO/l476Oñh4.20 I 9.l69h9ññ
Bagga, S. K., Gera, S., & Haque, S. N. (2022). The Mediating Role of Organizational culture: Transformational Leadership and Change Management in Virtual Teams. Asi‹i Pan i fi‹ Mon‹ipement Re iew, 28 2), I 20—131 . Sciencedirect.
https://doi.ore/1O.1O I 6/La9mrv.2022.07. 3
Balakrishnan, K., Brenner, M. J., Gosbee, J. W., & Schmalbach, C. E. (2019). Patient safety/quality improvement primer, part 11: Prevention of harm through rcint cause anal ysis and action (RCA2›. ni‹›i › np‹›i‹›p —Hens ›m New L Sut ge« , 161 6), 91 i — 92 I .
https://doi.ore/IO.1177/0 194a 99h I 9h7h6h3
Black, K. C., Snyder, N. A., Zhou, M., Zhu, Z., U ptegraft, C., Anirudh Chintal apani, & Orwoll, B. (2024). An electronic health record alert for inpatient COVl D- 19 vaccinations increases vaccination ordering and uncovers workflow inefficiencies. Applied
C’lini‹ ‹il In[orm‹iti‹ s, IS(0 I ).
https://doi.org/1O.1OFF/a-22ñO-63Oñ
Boikos, C., lmran, M., De Lusignan, S., Ortiz, J. R., Patriarca, P. A., & Mansi, J. A. (2022). Integrating electronic medical records and claims data for influenza vaccine research. Vo‹ ‹ inc.t, / 0 5), 727.
https://doi.org/1O.3390/vaccines IOOñO727
Brown, B., Gude, W. T., Blakeman, T., van der Veer, S. N., lvers, N., Francis, J. J., Lorencatto, F., Presseau, J., Peek, N., & Daker- White, G. (20 19). Clinical Performance Feedback Intervention Theory (CP-FIT): a new theory for designing, implementing,
and evaluating feedback in health care based on a systematic review and meta-s ynthesis of qualitative research.
Implement‹ition S‹ tend e, l4 I ).
https://doi.ore/ IO.1 I h6/st 3O I 2-0 l9-Ohh3-ñ
CDC. (2022, February 17). Vaccination Coverage among Adults in the United States, National Health Interview Survey, 2019-2020 1 CDC. Www.cdc.gov.
https://www.cdc.Nov/vaccines/imz-managers/coverage/adultvaxview/pubs-resources/vaccination-coverage-adults-2019-2020.html
CDC. (2023, August 25). .Se‹i.tonsil Flu Shot. Centers for Disease Control and Prevention.
https://www.cdc.gov/flu/prevent/flushot.htm
Cherian, T., Morales, K. F., M antel, C., Lambach, P., Al Awaidy, S., Bresee, J. S., C hunsuttiwat, S., Coulibaly, D., Feng, L., Hale, R.,
Madhi, S., Maltezou, H. C., Moore, K., Nguyen-Van-Tann, J., Omer, S., Poland, G., & Wicker, S. (2019). Factors and considerations for establishing and improving seasonal influenza vaccination of health workers: Repnrt from a WHO meeting, Januar y I 6-17, Berlin, Germany. Vn‹ ‹ inr, 37(43), 6255-626 I .
https://doi.org/1O.1O I 6/j.i’accine.20 I 9.07.079
Cieslowski, B., Brock, L., Richesson, R. L., Silva, S., & Kim, H. (2020). Optimization of nursing-specific flu alerts. C’IN.’ C’omputet s, In[ormoti‹s, Nursing, 38{9), I .
https://doi.org/IO.1097/cin.00000 0000 61 6
Coleman, D., & McLaughlin, D. (2019). Using simulated patients as a learning strategy to support undergraduate nurses to develop patient-teaching skills. British .lournol ofNiu sing, 28 20), I 300—1306.
httos://doi.orf/1O.1 296h/blon.20 I 9.2h.20.13
Communications, N. (202 l , November 16). Flu Vaccinations: HEDlS results du ring covid reveal disparities. NCQA.
https://www.ncGa.org/blog/flu -vaccinations-hedis-results-during-covid/
Cook, F., Glen, K., & Ngo, A. (2023). Service improvement for a dietetic-led radiologically inserted gastrostomy service using the Plan-Do-Study-Act (PDSA) cycle. C’lini‹ ‹il Nutriti‹›n Rpm .S‹ trna r, 5/.
https://doi.org/ IO.1O I 6/Lnutos.2023.Oh.O IO
Eboreime, E. A., Olawepo, J. O., Banke-Thomas, A., & Ramaswamy, R. (2020). Evaluating the design and implementation fidelit y of an adapted Plan-Do-Study-Act approach to improve health system performance in a Nigerian state. E ‹ilu‹ition urld Pt o pt‹inn Planning, 84, 101876.
htt ps://doi.org/10.10 l6/j.evalproqplan.2020.10 lS76
Figueroa, C. A., Harrison, R., C hauhan, A., & Meyer, L. (2019). Priorities and challenges for health leadership and workforce management globally: A rapid review. BMC’ Health Ser tree Reseor‹h, /9(1 ), I —1 I . Biomedcentral.
https://bmchealthservres.biomedcentral.com/articles/IO.1 Ih6/st 29 I 3-O I 9-40hO-7
Gates, A., Rahman, S., Sim, S., Pillay, J., Ismail, S. J., Tunis, M. C., Keto-Lambert, D., & Hartling, L. (202 I ). Health inequities related to vaccination: An evidence map of potentially influential factors and systematic review of interventions. Vo‹ ‹ inr, 39(29), 3825-3833.
https://doi.org/10.10 I 6/j.i’accine.202 I .OF.0ñ4
Geoghegan, S., O’Callaghan, K. P., & Offit, P. A. (2020). Vaccine Safety: Myths and Misinformation. Nrr›nriri:t in Mi‹v ohiolog v, 11 372).
https://doi.org/10.3389/fmicb.2020.00372
Grohskopf, L. A., Alyanak, E., Broder, K. R., Walter, E. B., Fry, A. M., & Jernigan, D. B. (201 9). Prevention and control of seasonal influenza with vaccines: Recommendations of the advisory committee on immunization practices — United States, 2019-20 Influenza Season. MMWR. Rev ommend iir›n.t nM firyr» r.t, 68 3), I —21 .
https://doi.ore/ IO.1 ññhñ/mmwr.rr6803a I
Grohskopf, L. A., Alyanak, E., Broder, K. R., Walter, E. B., Fry, A. M., & Jernigan, D. B. (20 19). Prevention and control of seasonal influenza with vaccines: Recommendations of the advisory committee on immunization practices — United States, 20 19-20 Influenza Season. MMWR. Rev ommend iir›n.t nM firyr» r.t, 68 3), I—21 .
https://doi.ore/ IO.1 ññhñ/mmwr.rr6803a I
Healthy People 2030. (n.d.). 1ncrease the proportion of people who get the flu vaccine every year — HD-09 – Healthv People 2030 I health.go . Health.gov.
https://health.Nov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase- proportion-people-who-get-flu-vaccine-every-year-iid-09
Jong, K. M., Sikora, C. A., & MacDonald, S. E. (2021 ). Childhood immunization appointment reminders and recalls: Strengths, weaknesses and opportunities to increase vaccine coverage. Puhli‹ He‹ilth, /94, 170— 175.
https://doi.org/1O.1O I 6/Lpuhe.202 I .02.034
Khairat, S., Xi, L., Liu, S., Shrest ha, S., & Austin, C. (2020). Understanding the association between electronic health record satisfaction and the well-being of nurses: Survey study. .IMIR Nursinp, 3{ I ), e13996.
https://doi.org/10.2196/13996
Kini, A., Morgan, R., Kuo, H., Shea, P., Shapiro, J., Leng, S. X., Pekosz, A., & Klein, S. L. (202 1). Differences and disparities in seasonal influenza vaccine, acceptance, adverse reactions, and coverage by age, sex, gender, and race. Van. ‹ inc, 40 I I ).
https://doi.orf/1O.1O I 6/1.vaccine.202I .04.0 13
Kopsidas, 1., Tsopela, G.-C., Maroudi-M anta, S., Kourkouni, E., Charalampopoulos, D., Sirogianni, A., Collins, M. E., Lourida, A., Kourlaba, G., Zaoutis, T. E., & Coffin, S. E. (2020). Increasing healthcare workers’ uptake of seasonal influenza vaccination in
a tertiary-care pediatric hospital in Greece with a low-cost, tailor-made, multifaceted strategy. Vo‹ ‹ inr, 38 29), 4609—46 15.
https://doi.org/1O.1O I 6/j.i’accine.2020.OF.02 I
Manyang, C., Stene, J., Pagel, E. M., & Niesen, C. (2020). A Balancing Act. Gar.stroentet olo pv Nursinp, Puhlish Ahe‹id r›/Prini(4).
https://doi.ore/1O.1097/sqa.OO OOOO OOO446
McGee, J. (2021). 1ncreasing vaccination rates in pregnancy using a multifaceted approach including patient education and reminder/recall interventions. E ident e-B‹ised Pt ‹u. tire Prr›Jr‹ r firyr» r.t.
https://scholar.i’alpn.edu/ebpr/176/
Moffett, J., Mitchell, T., & Simmons, V . (2021). A survey of primary care providers’ strategies to affect influenza vaccination rates.
MSN Reseur‹ h Prr›Jr‹ r.t.
https://athenacommons.muw.edu/msn-projects/433/
Mu kwato, P. K. (2020). Implementing evidence based practice nursing using the PDSA model: Process, lessons and implications.
Munna, A. (2021 ). Strategic management, leadership and staff motivation: Literature review. Intern‹ition‹il Edna ction wd C’ultut e Studies, 1 1), 2 I —29.
https://repository.uwtsd.ac.uk/id/eprint/lSñ7/
Near, A. M., Tse, J., Young-Xu, Y., Hong, D. K., & Reyes, C. M. (2022). Burden of influenza hospitalization among high-risk groups in the United States. BMC’ Health Ser i‹ re Rrsror‹ h, 22 1), 1 209.
https://doi.ore/10.1 I86/s 1 29 I 3-022-0hñ86-v
Perl, T. M., & Talbot, T. R. (2019). Universal influenza vaccination among healthcare personnel: Yes we should. Rpm Forum In[e‹ tion.t Disr‹zses, 6(4).
https://doi.ore/1O.1093/ofid/ofzo96
Pyne, J. M., Seal, K. H., Manuel, J. K., DeRonne, B., Karen Anderson Oliver, Bertenthal, D., Esserman, D., Purcell, N., Beth Ann Petrakis, & A. Rani Elw y. (2023). Developing and testing a COV lD- 19 vaccination acceptance intervention: A pragmatic trial comparing vaccine acceptance intervention vs usual care — Rationale, methods, and implementation. C’ontemporurv C’lini‹‹if Trials, 133, 107325—107325.
https://doi.org/1O.1O I 6/Lcct.2023.1 O732ñ
Reifferscheid, L., Kiely, M. S., Lin, M. S. N., Libon, J., Kennedy, M., & MacDonald, S. E. (2023). Effectiveness of hospital-based strategies for improving childhood immunization coverage: A systematic review. Vn‹ ‹ inr, 4/(36), 5233-5244.
https://doi.org/1O.1O I 6/j.i’accine.2023.07.O36
Schouten, B. C., Cox, A., Duran, G., Kerremans, K., Banning, L. K., Lahdidi oui, A., van den Muijsenbergh, M., Schinkel, S., Sungur, H., Suurmond, J., Zendedel, R., & Krystallidou, D. (2020). Mitigating language and cultural barriers in healthcare communication: Toward a holistic approach. Porirnr Edna ‹ition and C’oun. elinp, 103 1 2), 2604-2608.
https://doi.org/10.10 I 6/}.pec.2020.OF.00 I
Schouten, B. C., Cox, A., Duran, G., Kerremans, K., Banning, L. K., Lahdidi oui, A., van den Muijsenbergh, M., Schinkel, S., Sungur, H., Suurmond, J., Zendedel, R., & Krystallidou, D. (2020). Mitigating language and cultural barriers in healthcare communication: Toward a holistic approach. Patient Edna ction and C’ounsrling, 103 1 2), 2604-2608.
https://doi.ore/1O.1O I 6/Lice.2020.OF.OO I
Spelman, J. F., Kravetz, J. D., Bastian, L., & Ruser, C. (2022). Addressing covid- 19 vaccine acceptance within a large healthcare system: A population health model. .fournol r›{G enerul Internal Media inc, 37.
https://doi.org/10.1007/st I 606-021-07353-9
Szilagyi, P. G., Albertin, C., Casillas, A., Valderrama, R., Duru, O. K., Ong, M. K., Vangala, S., Tseng, C.-H., Rand, C. M., Humiston, S. G., Evans, S., Sloyan, M., & Lerner, C. (2020). Effect of patient pnrtal reminders sent by a health care system on influenza vaccination rates. .IAMA Intern‹il Media inc, 180 7), 962.
https://doi.org/IO.lOO I /jamainternmed.2020.1602
Vankar, P. (2024). Flu ro‹ ‹ inoiir›n iorrs 6v yrar wd ogr t/ S. 2014-2022. Statista.
https://www.statista.com/statistics/h6 I l76/flu- vaccine-coverage-by-age-us/#:-:text=ln°/e20the°/e20United°/e20States°/e2C°/e20influenza
Vasallo, M. D. E., Berjon, M. F. D., Riolobos, C. G., Zoni, A. C., Aréjula Torres, J. L., Sanchez-Perruca, L., & Astray-Mochales, J. (2019). Effect of mobile phone text messaging for improving the uptake of influenza vaccination in patients with rare diseases. Vo‹ ‹inc, 37 36), 5257-5264.
https://doi.org/1O.1O I 6/j.i’accine.20 I 9.07.062
Werk, L. N., Diaz, M. C., Cadilla, A., Franciosi, J. P., & Hossain, M. J. (201 9). Promoting adherence to influenza vaccination recommendations in pediatric practice. .Iourn‹il of Pt im‹it v C’‹it e d: C”ommunitv He‹ilth, 10, 215013271985306.
https://doi.org/10.1177/21 TO1327 l9Sñ 306 I
Wijesundara, J. G., lto Fukunaga, M., Ogarek, J., Barton, B., Fisher, L., Preusse, P., Sundaresan, D., Garber, L., Mazor, K. M., & Cutrona, S. L. (2020). Electronic health record portal messages and interactive voice response calls to improve rates of earl y season influenza vaccination: Randomized controlled trial. .min nol r›/ Mrdi‹of Intrt nat Rrsror‹h, 22{9), e 1 6373.
https://doi.ore/10.2 I 96/16373
Wijesundara, J. G., lto Fukunaga, M., Ogarek, J., Barton, B., Fisher, L., Preusse, P., Sundaresan, D., Garber, L., Mazor, K. M., & Cutrona, S. L. (2020). Electronic health record portal messages and interactive voice response calls to improve rates of early
season influenza vaccination: Randomized controlled trial. .Iourn‹il r›/ Media ‹il Internet Reseur‹ h, 22{9), e 16373.
https://doi.ore/10.2 I 96/16373
Zajac, S., Wcinds, A., Tannenbaum, S., Salas, E., & Holladay, C. L. (202 I ). Overcoming challenges to teamwork in healthcare: a team
effectiveness framework and evidence-based guidance. Nrr›nriri:t in C’r›mmuni‹ orir›n, 6{ 1).
https://doi.org/IO.3359/fcomm.202 I .60644a
Appendix A
Root Cause Analysis
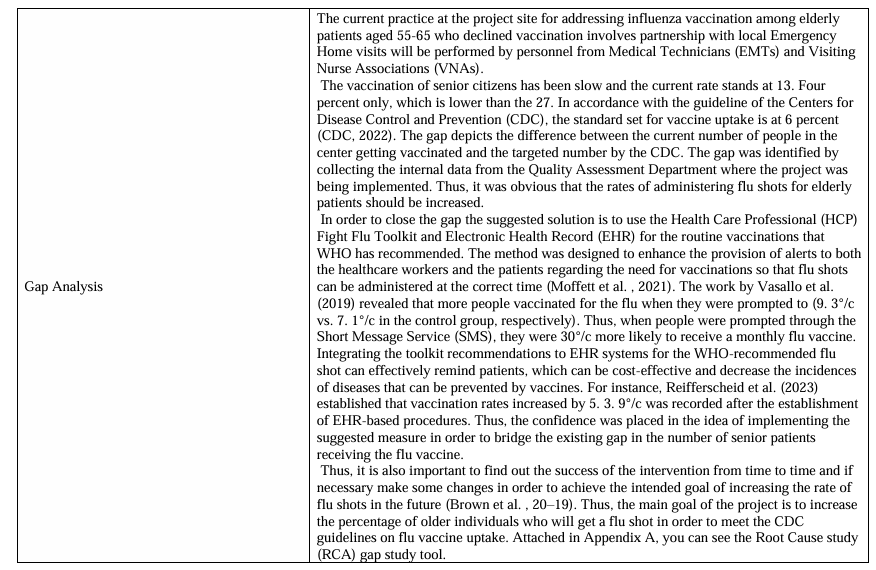
Root cause analysis (RCA) is one of the effective methods used in healthcare to determine the causes of adverse events. This allows the healthcare professionals to design preventive measures to avoid such occurrences in the future and ensure that patients are protected (Balakrishnan et al. , 2019).
It was noted earlier that with RCA it is possible to find out why there is a gap in the number of people who receive flu shots among the 55 to 65-year-olds. Another possible cause of the gap could be inadequacy of the health care facility in communication and warning systems (Jong et al. , 202 I).
The present approach of having EMTs and VNAs to go to the homes of patients may not effectively convey the message to the patients the importance of getting a flu vaccine. These methods may also have problems that cannot be easily explained to people which can be discouraging and slows the process of vaccination.
NURS FPX 9100 Assessment 6 Project Charter
Another possible cause could be that the healthcare workers do not rely on the EHR in the manner that is expected (Khairat et al. , 2020). If they are not linked, perhaps the different healthcare workers may not be able to link and follow up on the prior vaccine information. This could be due to the fact that there is a lack of knowledge on the new methods of immunization because the previous methods were manual.
One of the causes is that the senior patient already knew or believed that he or she required a flu shot. Some patients have been targeted to get vaccinated, yet some patients may refuse to get vaccinated since they hold certain beliefs about the vaccines, or they may be too idle to get the flu vaccine (Geoghegan et al. , 2020).
By employing the HCP Fight Flu Toolkit and EHR that is encouraged by WHO, patients’ vaccination rates can be increased, as well as identifying the reasons for not getting vaccinated among the elderly. This can be achieved through enhancing the manner of communication, enhancing the reminder systems and ensuring that the patients are involved and informed.
If you need complete information about class 9100, click below to view a related sample:
NURS FPX 9100 Assessment 5 Virtual Check-in 2
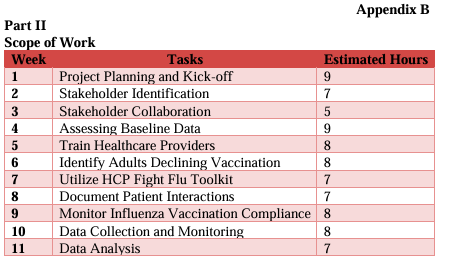
Appendix B