- NURS FPX 6016 Assessment 1 Adverse Event or Near-Miss Analysis.
Adverse Event
Adverse events (AE) often happen in any medical framework; at least one out of ten patients are affected. An Adverse Event is a harmful and negative result that occurs when a patient has been given medical care (Skelly, 2022). Examples of Adverse Events incorporate, yet are not restricted to, falls, medication goofs, hospital-acquired infections, and astonishing deaths. Adverse Events can be classified as either preventable or unpreventable. Nonetheless, profound leap analyses should be done on all events to conclude the factors leading to the event and how this can be avoided later.
A 73-year-more-established person was brought to the ED after her son called 911, stating his mother’s mental status had changed and she was lethargic. Upon arrival at the Hospital, the patient was alert and angry she was there and became verbally abusive and combative towards staff individuals. She attempted to leave the ED on various occasions and had to be restrained by security and nursing staff. Upon evaluation by the MD, the patient was placed under a Baker Act, a 72-hour involuntary hold.
After being admitted to the inpatient floor for 2 days, various evaluations by the internal Hospitalist and Psychiatrist, and incessant communication with the patient’s son, the decision was made to lift the patient’s Baker Act. The patient, nevertheless, was hanging out there all the while to leave the Hospital, although the Nursing and Case Management staff was dealing with placement at an assisted dwelling facility.
Preventing High-Elopement Risks
After shift change one evening, the patient eliminated all her hospital attire and identification, including her IV access, ran towards the nursing unit’s back staircase, and left the Hospital. The patient bypassed security by leaving an unaided exit and running into the road. Because it was 9 P.M., the roads were exceptionally dark and under low light. The patient attempted to go across the road, where she was unfortunately hit by a get truck and passed on.
The nursing unit saw the patient absent within 10-15 minutes of her disappearance. A code Reverberation was called overhead immediately, and all staff continued to search for the patient. During the search, a security officer informed the unit’s manager that trauma had recently become acquainted with the ED, which matched the missing patient’s description. The assigned RN and Nursing Manager saw the trauma to ensure their missing patient.
This event shows an adverse event that could have been prevented, assuming the patient was still under her Baker Act with a 1:1 sitter, considering that a safety sitter was still in place because of the patient’s high elopement risk. This event profoundly saddened the Nursing staff and advanced a full-scale analysis of patients who present with a high-elopement hazard and how events as such could be avoided starting now and into the foreseeable future.
Explore our assessment NURS FPX 6016 Assessment 3 for more information.
Analysis of Missed Steps Related to the Adverse Event
Patients under the Baker Act (BA52) in a hospital or other healthcare facility should be under 1:1 direct observation, remove all sharp and unnecessary medical gear from the room, and be identified with alternate shaded patient outfits and socks. NURS FPX 6016 Assessment 1 Adverse Event or Near-Miss Analysis is essential for determining an Elopement Hazard, a patient familiar with their medical condition and the dangers and advantages of searching for treatment yet chooses to leave without authorization or an approved discharge.
An absconded patient may be in danger of serious harm. When a Baker Act patient leaves a facility without authorization and staff awareness, this is considered an elopement. Close 1:1 supervision is regular by staff for patients who are seen as an elopement risk (Castellanos, 2014). Above all else, after the patient’s Baker Act was repudiated, the assigned RN ought to have assessed the patient and her medical/social history to pick the patient’s elopement status.
NURS FPX 6016 Assessment 1 Adverse Event or Near-Miss Analysis
Regardless, because this was not essential at the Hospital, and the unit was understaffed due to Coronavirus, the RN bypassed doing so and continued to treat other patients. According to Joint Commission sentinel event statistics, the primary contributors to elopement are patient assessment and team communication breakdowns. Protecting patients from elopement chances anticipates that attention should be paid to preventive measures through assessment and elopement precautions and appropriate intervention after elopement (Gerardi, 2017).
Addressing Elopement Risk Protocols
The unfortunate scenario shows that no strategy or methodology was in place for patients who were considered elopement dangers or for assessing a patient’s elopement risk status. The RN would never have realized the patient’s elopement risk at any point, except assuming the past shift had mentioned it on the off chance that she had assessed the patient first.
Various framework factors, such as communication, lack of strategy, framework, and training, affected the adverse event. If such factors had been ideal, the patient would have been under the supervision of a safety sitter or attendant and, therefore, would never have left unauthorized.
Implications of the Adverse Event on Stakeholders
Stakeholders in healthcare play a significant role in financing, support, strategic direction, solutions, and the overall quality of their healthcare framework. While patients and their family individuals are the immediate casualties of adverse events and healthcare professionals the second, the stakeholders are the third. Various stakeholders are responsible for guaranteeing that patient care is safely conveyed and that patients are not harmed, including society overall, patients, clinicians including physicians and attendants, educators, administrators, researchers, professional bodies, legislatures and legislative bodies, and accrediting agencies (Cho et al., 2020)
Analyzing an adverse event is the initial step the stakeholders should take to determine the impact on the patient, family, and organization. The stakeholders depend on detail, and charts concentrate on approaches to observe adverse events that have already happened. The emphasis is on analyzing a subset of adverse events to pick stowed away drivers and see improvements in care processes, ultimately dealing with patient safety (Patient safety: Achieving another standard for care).
Adverse events are based on Healthcare organizations from accreditation agencies like JACHO and ACHA. Stakeholders are considered responsible for the analysis and resolution following adverse events. In this case, stakeholders should create a strategy encompassing patient safety and elopement chances. This elaborates all key stakeholders, administrators, nursing leaders, and various clinical teams to develop an Elopement Hazard Decision Tree – which would assist with seeing elopement risk patients and establish a safety plan for their hospitalization and another security framework, which zeroed in on leave places and confined access entryways.
Evaluation of Quality Improvement Technologies
Following the organization’s adverse event, the principal evaluation was done on the Hospital’s security framework. Although one-to-one monitoring is robust at preventing elopements and wandering and the wounds that often result (like falls by additional seasoned patients or suicides by behavioral health patients), it is exorbitant. It can drain the assets of a security department. Fortunately, innovation can help. Sitters can utilize telemonitoring or remote monitoring to find patients in danger via surveillance cameras. Additionally, Video surveillance is beneficial when an elopement happens (Hattersley-Gray, 2018).
The organization acknowledged that various staircases were unalarmed and accessible to anyone. Also, cameras didn’t zero in on these entryways because they are rarely utilized.
The security and IT team picked in efforts to increase patient safety; the entryways would be badged. Access only, allowing only staff individuals to access, and at least one camera would be adjusted to zero in on the entryways.
To guarantee the new safety efforts are viable and workable, steps, for example, 1, should be taken: Realize security-related Police and carry out reasonable and appropriate safeguarding strategies; 2. Ensure your staff know the arrangements and your training is accounted for; 3. Guarantee the quality of episode documentation; 4. Respond to investigations rapidly (Smith). The new turn of events and the training and follow-up encompassing new safety efforts are essential to a viable plan.
Relevant Metrics of Quality Improvement Plan
Measuring patient safety has always been debatable amongst health organizations and stakeholders. There are various strategies to measure messes and adverse events, for example, dreariness and mortality conferences, malpractice claims analysis, mistake announcing frameworks, administrative data analysis, chart outline, Emrs, observation of patient care, and clinical surveillance. The AR utilizes dashboards that follow standard formats for event announcements.
NURS FPX 6016 Assessment 1 Adverse Event or Near-Miss Analysis
They report on unambiguous events like episodes, near misses, and unsafe conditions. Two arrangements of interactive hospital safety event dashboards are introduced: the Data Submission Summary Dashboard, which gives a significant level outline of the repeat of patient safety events revealed, and the Patient Safety Event Dashboards, which incorporate a nonexclusive section that offers an outline of the numbers and categories of various patient safety event reports, and dashboards that portray in greater profundity the patient harm experienced because of unequivocal safety events (NPSD Dashboards, 2021).
Regardless, when adverse events can be measured, an additional layer of controversy concerns assuming that the event was preventable. In the seminal examinations that formed the basis of To Goof Is Human, experienced clinicians often disagreed on whether a mistake was preventable. Contrasts in definitions of goofs account for a portion of the wide variation in estimates of the proportion of hospitalized Zedd patients who experience preventable harm, which ranges from about 12% among Medicare patients in the 2010 Office of the Inspector General survey to nearly 33% in another report (Measurement of Patient Safety).
Outline for a Quality Improvement Initiative
In addition to the new safety efforts and partnerships from JACHO and ACHA, the organization has adopted the Elopement Hazard Decision Tree. This tool assists the Medical caretaker in determining whether a person is in danger of elopement from the Hospital while allowing the patient to reach their generally elevated attainable degree of physical, mental, and psychosocial thriving. The tool was utilized swiftly by each patient admitted to the ED upon a change in mental status.
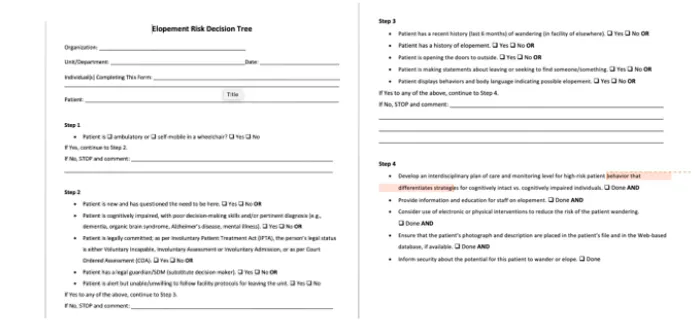
Assuming the patient is considered to be an elopement risk, an interdisciplinary plan of care and monitoring should be created. This incorporates nursing staff, physicians, case management, and family participation. Electronic (security frameworks) or physical (safety attendant) interventions should be utilized to decrease the chance of the patient wandering.
Implementing Elopement Risk Protocols
The Administrative boss and security team should be informed about the elopement risk patient information. After 90 days of utilizing the Elopement Chance decision tree, the Hospital identified 73 patients in danger of elopement, provided 1:1 safety attendants 91% of the time, and received great feedback from many family members who felt their friends and family were “safer under the new arrangement.”
A QI study was done at a Pediatric Behavioral Health Facility in a similar attempt to decrease elopementsUtilizinging a quality improvement (QI) approach, we aimed to reduce the repeat of significant safety events (SSEs) in this population by targeting modifiable gamble factors and astandardizinging care. Key interventions incorporated improving the Pediatric Behavioral Health Safety Protocostandardizinging the patient safety search and implementing a daily Safety Pack.
Using QI strategy to further encourage safety for adolescents admitted after an implosion attempt provoked a substantial and sustainable reduction in the rate of SSEs at our institution” (Noelck et al., 2015). While implementing Quality Improvement Plans, the organization should have full assistance from its stakeholders, healthcare professionals, and innumerable clinical and allied team members. Teamwork will enable the organization to cultivate further framework factors and the quality of approaches and strategies to prevent future adverse events.
Conclusion
Preventable and Non-preventable adverse events affect organizations and their families. NURS FPX 6016 Assessment 1 Adverse Event or Near-Miss Analysis plans, for example, increased safety efforts and the Elopement Chance Decision Tree adaptation, are based on seeing events before they can. With the proper education and training, healthcare professionals can provide their patients with the safest, most magnificent care.
References
Castellanos, D. (2014, June 1). Policy title: Psychiatry emergency: Involuntary … Retrieved February 28, 2022, from https://policies.medicine.fiu.edu/Documents/Psychiatry%20Emergency%20Involuntary%20Examination%20Hospitalization%20Baker%20Act.pdf
Cho, I., Lee, M., & Kim, Y. (2020, August). What are healthcare stakeholders’ primary patient safety concerns: A mixed-method study of web-based text. International journal of medical informatics. Retrieved March 21, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7198194/
Gerardi, D. (2017, December 1). Elopement. Patient Safety Network. Retrieved February 28, 2022, from https://psnet.ahrq.gov/web-mm/elopement
Hattersley-Gray, R. (2018, April 9). Responding to elderly patient elopement and wandering: Part 2. Campus Safety Magazine. Retrieved February 28, 2022, from https://www.campussafetymagazine.com/news/elderly-patient-elopement-wandering/
Measurement of Patient Safety. Patient Safety Network. (2019, September 7). Retrieved February 28, 2022, from https://psnet.ahrq.gov/primer/measurement-patient-safety
Noelck, M., Velazquez-Campbell, M., & Austin, J. P. (2019). A Quality Improvement Initiative to Reduce Safety Events Among Adolescents Hospitalized After a Suicide Attempt. Hospital pediatrics, 9(5), 365–372. https://doi.org/10.1542/hpeds.2018-0218
NPSD Dashboards. Content last reviewed August 2021. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/npsd/data/dashboard/index.html
Patient safety: Achieving a new standard for care. National Academies Press: OpenBook. Page (n.d.). Retrieved February 28, 2022, from https://www.nap.edu/read/10863/chapter/10#202
Skelly, C. L. (2022, February 9). Adverse events. StatPearls [Internet]. Retrieved February 28, 2022, from https://www.ncbi.nlm.nih.gov/books/NBK558963/
Smith, T. (n.d.). Healthcare Security Consultants, Inc.. Retrieved February 28, 2022, from https://healthcaresecurityconsultants.com/pdfs/Brochure.pdf
