NURS FPX 8022 Assessment 1 Sample FREE DOWNLOAD
NURS FPX 8022 Assessment 1 Using Data to Make Evidence-Based Technology Recommendations
Student name
Capella University
NURS-FPX8022 Nursing Technology and Advanced Healthcare Information Systems
Professor Name
Submission Date
Using Data to Make Evidence-Based Technology Recommendations
Technology recommendations are vital in the healthcare sector, where data is used to formulate a decision that will allow a healthcare institution to understand how it can invest in technology, which will directly translate to patient outcomes and operational effectiveness. Scientific analysis of clinical outcomes, safety measurements, and workflow could assist the leaders in selecting the technologies with promising outcomes rather than on the vendor’s assertion.
The evidence-based strategy minimizes the risk of implementation, optimally utilizes resources, and connects the newly introduced technologies with the quality improvement objectives within the organization. The adoption of innovations resulting in better care delivery and possessing a measurable value and payoff will eventually be implemented through informed decision-making (Lyu, 2025). The main area that will be evaluated in the assessment will be the utilization of technology in the real life situations and the utilization of performance information in the creation of evidence-based technology advice.
Evaluation of Technology in Use
Healthcare organizations need to engage in performance benchmarking against national standards as a continuous process that is aimed at optimizing patient outcomes and identifying important areas of improvement. The problem with performance lapses at the Medical University of South Carolina University Medical Center is severe because the number of patient falls per 1,000 patient days is 0.774 as compared to 0.000 in the top performers, and this could indicate that there is a severe patient safety problem (Leapfrog, n.d.).
The institution has a medication communication score of 74, compared to the 88 score of the highest-ranked hospitals, demonstrating that the institution had not effectively taught patients on medication regimens and adverse effects (Leapfrog, n.d.). The performance in communication on discharge is 82, which is, on average, lower than the national average, and an improvement in comparison to other low-performing facilities with 67, and standardization opportunities have a chance (Leapfrog, n.d.). Introduction of strategic technology and general staff training programs is a crucial measure toward achieving perfection in patient safety and communication levels.
Interactive patient education systems and automated medication dispensing systems can play a significant role in increasing medication communication and discharge planning at a healthcare facility. The technology interventions will be able to enable the medical professionals to give standardized medication counseling and discharge training through touchscreen displays with visual learning materials (Mason et al., 2022).
The systems eliminate the variations in communication plans and specify the procedures of systematic patient awareness of drug compliance and post-discharge practices (Osei et al., 2025). Interventions that involve the use of technology to standardize the process of medication and discharge communication will enhance patient safety outcomes and reduce the occurrence of preventable adverse events that are preventable.
The obstacles to the implementation of the new communication technologies in medical facilities have been overwhelming as the organizations fight with the competing institutional concerns, the lack of resources, and the human aspects of the implementation process. The resistance of the staff to interactive systems of educating patients is usually linked to the fear of the increased workload demands and the absence of knowledge about the digital interface (Provenzano et al., 2024).
The financial deficiency, particularly among smaller healthcare facilities, restrains the procedure of buying automated medication delivery systems and the investments that are necessary to educate the staff. The complexity of integration that will be created at the level of technology, which involves integrating the new communication platforms with the current electronic health records systems, could disrupt the workflow and clinical processes of the current system.
The issue of digital gaps in healthcare may grow due to the fact that the patients who lack technological literacy will face difficulties with the efficient use of the touchscreen-based education systems (Bitomsky et al., 2025). The two key elements that determine the successful implementation of technology in different healthcare environments are the planning of strategic implementation and long-term administrative support.
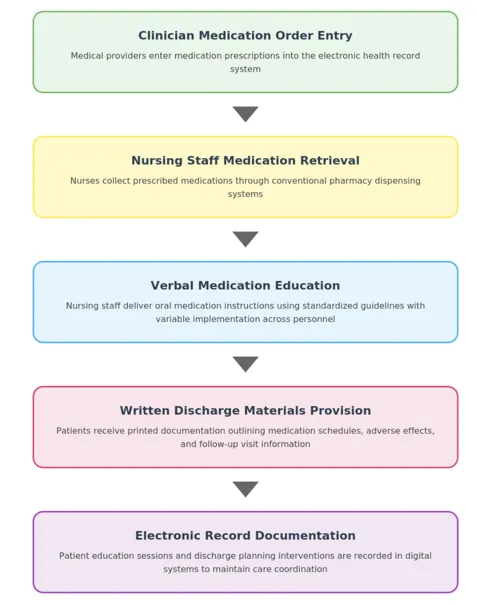
The current process of medication communication and discharge of the MUSC entails the contribution of the providers who make medication requests in the patient files, and the nurses who receive the medications according to the regular pharmacy delivery systems. The nurses offer verbal medication education in standard protocols, but the quality of delivery differs with how individual practitioners deliver it and time constraints. The efficiency of healthcare delivery systems will be achieved when nurses undertake the whole process of educating patients with the aid of technology (Altmiller and Pepe, 2022).
Structured methodologies should be included in the best communication practices that would address the diverse preferences and needs of patients in terms of learning (Hickey et al., 2023). The patient is typically provided with the discharge instructions in written format, in which the schedules of the drug usage, adverse effects, and follow-up appointments are mentioned. The continuity of care is developed by means of documentation in the electronic health record system that provides long-term records of patient education contacts and discharge planning activities. The existing workflow design is presented in Appendix A.
Patient Safety Areas Identified
Healthcare facilities have two primary assessment frameworks, such as Leapfrog safety ratings and Medicare comparison tools, as means of performance evaluation. Leapfrog is a terminology based on letter grades (A-F) regarding the overall safety indicators, which include protocol compliance, infection control, and clinical outcomes (Razick et al., 2024). The measures provided by Medicare look at a broader range of healthcare delivery and patient satisfaction issues, which can be studied in comparison to identify the provider (CMS, 2023).
These three basic purposes of the evaluation systems are to foster operational transparency, to strengthen quality improvement programs, and to present the consumers with the evidence-based information to make informed healthcare choices. The standardized monitoring systems deploy similar evaluation requirements that, when combined, foster the quality of medical care by giving it greater accountability and informed choice of the consumer.
In many of the performance measures at the discussed healthcare facility, there are severe gaps in the indicators of patient safety and quality of communications. The MUSC demonstrates great, shocking outcomes in terms of falls prevention performance, with falls per 1,000 patient days of 0.774 falls per 1,000 patient days being a considerably higher performance than the national average of 0.38 score and the benchmark of 0.000 falls per 1,000 patient days (Leapfrog, n.d.).
Even though medication communication scores (74) and discharge communication scores (82) are considered to be satisfactory levels of performance, they are much lower in comparison to the leading facilities, where the scores are rated at 88 and 94, respectively (Leapfrog, n.d.). The differences in the performance raise certain fundamental questions whether the medical center works to create a complex of overall standards of patient safety and offer evidence-based interventions in teaching the patients.
Table 1
Medical University of South Carolina University Medical Center Score Comparison
Categories | Facility Score | Top Facility Score | Average Facility’s Score | Lowest Center’s Score |
Injuries due to Patient Falls | 0.774 | 0.000 | 0.338 | 1.748 |
Communication about Medicine | 74 | 88 | 74.64 | 59 |
Communication about Discharge | 82 | 94 | 85.48 | 67 |
Note. The statistics demonstrate the Leapfrog safety grade ratings of the Medical University of South Carolina University Medical Center concerning the set industry standards. In the case of patient fall measurements, low numbers reflect better performance, whereas in communication measurements, high scores reflect excellent performance. The Leapfrog Hospital Safety Grade database (Leapfrog, n.d.) was used to retrieve data.
The MUSC Medical Center shows inconsistent results in terms of Medicare quality indicators, which show its strong and weak sides, as well as opportunities to improve. The facility has a general rating of 4 stars and a 3-star patient survey rating (Medicare, n.d.). The medical center has outstanding results in colonoscopy follow-up care at 98% as compared to the national average of 92, stroke care at 88% as compared to the national average of 70, but lags in sepsis management at 48% as compared to the national average of 64, and suffers the problem of efficiency in the emergency department (Medicare, n.d.).
The institution has a strong rate of influenza vaccinations, with 81 out of 100 patients being vaccinated, which is higher than the national vaccine rate of 78, and better results in several infection prevention measures, such as central line-associated bloodstream infection and catheter-associated urinary tract infection (Medicare, n.d.). Operations in the emergency department show alarming results of delays, with the average length of visits amounting to 216 minutes versus 195 minutes in similar high-volume hospitals across the country (Medicare, n.d.). These results highlight the most essential issues requiring increased emergency department workflow optimization and sepsis recognition guidelines as an element of the healthcare delivery system.
The data of healthcare performance show that there is a significant variability in operational activities of major academic medical Centres in differing clinical areas. Cleveland Clinic has a 57-percent gap in medication communication as compared to Mayo Clinic, which has an enhanced 66-percent performance, and both hospitals report sepsis management issues that are below the national average of 64 percent at 51 and 65 percent, respectively (Medicare, 2025a; Medicare, 2025b).
The statistics of the EDs indicate that the Cleveland Clinic has alarming data of 196 minutes as an average wait duration versus the long 203 minutes in the Mayo Clinic (Medicare, 2025a; Medicare, 2025b). Compared to the best 90 percent of the Cleveland Clinic, Mayo Clinic is performing poorly at 50 percent compared to the 78 percent national average (Medicare, 2025a; Medicare, 2025b). Medicare spending indices indicate that there are differences in fiscal stewardship at 0.94 and 0.99, respectively, and a national 0.99 average (Medicare, 2025a; Medicare, 2025b). The broad-based quality improvement initiatives are still needed to continue developing patient care excellence and operational efficacy within large healthcare facilities.
Recommended Technology Implementation
To addreSince the performance gaps that have been identified, MUSC must resort to the use of interactive patient education tablets fitted with automated bedside medication dispensing systems. It has been demonstrated by the existing evidence that healthcare facilities that implemented the integrated technologies have improved the medication errors by a significant margin, and they have also elevated the patient comprehension (Pal et al., 2021).
The current score of the organization on medication communication is 74, the rate of falls is 0.774 per 1000 patient days, and the discharge communication score of 82 points should be included in the personalized multimedia content, multilingual system, as well as the real-time documentation capabilities (Leapfrog, n.d.). The quality improvement processes might be made easier by the automated feedback collection systems, presented as touchscreen interfaces, and, consequently, the overall level of patient satisfaction is likely to go up (Ong et al., 2020). The entire technology strategy complies with the existing electronic health record infrastructure completely and responds to the specific patient education, access, and safety gaps across the healthcare continuum.
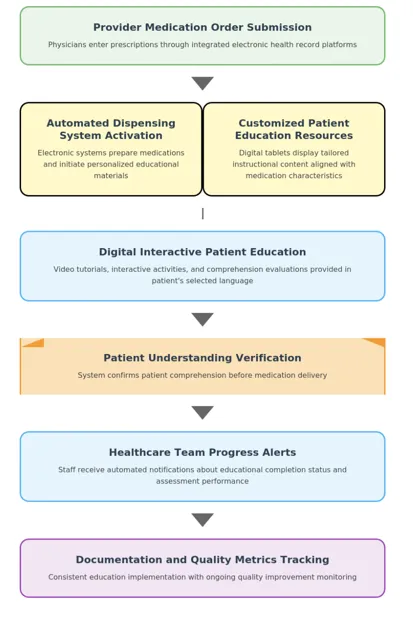
Following the incorporation of technology, the processes of medication management have been transformed into an interactive digital workflow that allows patients to be actively engaged in the process of encounter with treatment instead of the conventional channels of verbal communication. An order is made by physicians through integrated computerized systems, registered and, simultaneously, activates automated dispensing devices to fill drugs and offer personalized educational information to the patient at the bedside (Jungreithmayr et al., 2021).
The e-system offers individual video demonstrations, interactive simulations, and understanding assessments in the language of preference of the patients (Medel et al., 2024). The level of patient engagement before the administration of medication is monitored by the clinical staff, and the system notifies patients about passing the educational modules and the outcomes of the knowledge test. The safety is encompassed in a comprehensive education course and patient confirmation of understanding of the means of administration and potential side effects (Ricciardi and Cascini, 2020). The approach eliminates the diversity of communication, the homogenization of the way of providing patient education, and establishes indicators of ongoing quality enhancement monitoring. The simplified workflow is presented in Appendix B.
Conclusion
The introduction of evidence-based technology has been listed among the fundamental strategies that a healthcare organization can rely on in a bid to achieve sustainability in clinical excellence and operational effectiveness. The analysis demonstrates that automated medication dispensing systems and digital platforms of patient education have a significant impact on improving medication safety measures and communication processes.
Through the systematic application of the full-scale quality measures of Leapfrog and Medicare comparison databases, the healthcare facilities will be in a position to identify the performance gaps in a systematic manner, as well as implement the respective technological interventions. The approach enables the medical centers to correct some of the areas of weakness in the operations, while also enhancing quantifiable quality. Lastly, the changes in the quality of care delivery and patient satisfaction rates are sustainable because of the technology recommendations that are made, based on the data.
Explore Next Assessment: NURS FPX 8022 Assessment 2
Struggling with NURS FPX 8022 Assessment 1? Get step-by-step guidance to master technology recommendations and improve grades.
Step By Step Instructions To Write
NURS FPX 8022 Assessment 1
Contact us to receive step-by-step instructions to write this assessment.
Instruction file for 8022 Assessment 1
Contact us to get the instruction file.
Scoring Guide for 8022 Assessment 1
Contact us to get the Scoring file.
References For
NURS FPX 8022 Assessment 1
Altmiller, G., & Pepe, L. H. (2022). Influence of technology in supporting quality and safety in nursing education. Nursing Clinics of North America, 57(4), 551–562. https://doi.org/10.1016/j.cnur.2022.06.005
Bitomsky, L., Pfitzer, E., Nißen, M., & Kowatsch, T. (2025). Advancing health equity and the role of digital health technologies: A scoping review. BioMed Journal Open, 15(6), e099306. https://doi.org/10.1136/bmjopen-2025-099306
CMS. (2023, September 6). Hospital quality initiative public reporting | CMS. Cms.gov. https://www.cms.gov/medicare/quality/initiatives/hospital-quality-initiative/hospital-compare
Hickey, E., Man, B., Kaila, Lockhart, S., Duffecy, J., & Morris, M. A. (2023). Preferred communication strategies for people with communication disabilities in health care encounters: A qualitative study. Journal of General Internal Medicine, 39(5), 790–797. https://doi.org/10.1007/s11606-023-08526-4
Jungreithmayr, V., Meid, A. D., Bittmann, J., Fabian, M., Klein, U., Kugler, S., Löpprich, M., Reinhard, O., Scholz, L., Zeeh, B., Bitz, W., Bugaj, T., Kihm, L., Kopf, S., Liemann, A., Wagenlechner, P., Zemva, J., Benkert, C., Merle, C., & Roman, S. (2021). The impact of a computerized physician order entry system implementation on 20 different criteria of medication documentation—A before-and-after study. BioMed Central Medical Informatics and Decision Making, 21(1), 279. https://doi.org/10.1186/s12911-021-01607-6
Leapforg. (n.d.). Medical University of South Carolina University Medical Center – SC – Hospital Safety Grade. Hospitalsafetygrade.org. https://www.hospitalsafetygrade.org/h/medical-university-of-south-carolina-university-medical-center
Lyu, G. (2025). Data-driven decision making in patient management: A systematic review. BioMed Central Medical Informatics and Decision Making, 25(1), e239. https://doi.org/10.1186/s12911-025-03072-x
Mason, M., Cho, Y., Rayo, J., Gong, Y., Harris, M., & Jiang, Y. (2022). Technologies for medication adherence monitoring and technology assessment criteria: Narrative review. Journal of Medical Internet Research MHealth and UHealth, 10(3), e35157. https://doi.org/10.2196/35157
Medel, D., Bonet, A., Herrera, M. J., Sevilla, F., Vilaplana, J., Cemeli, T., & Roca, J. (2024). Interactive virtual simulation case: A learning environment for the development of decision-making in nursing students. Teaching and Learning in Nursing, 20(1), 60–68. https://doi.org/10.1016/j.teln.2024.08.002
NURS FPX 8022 Assessment 1 Using Data to Make Evidence-Based Technology Recommendations
Medicare. (2025a). Find healthcare providers: Compare care near you | Medicare. Medicare.gov. https://www.medicare.gov/care-compare/details/hospital/100151/view-all?city=Jacksonville&state=FL&zipcode=&measure=hospital-timely-and-effective-care
Medicare. (2025b). Find healthcare providers: Compare care near you | Medicare. Medicare.gov. https://www.medicare.gov/care-compare/details/hospital/360180/view-all?city=Cleveland&state=OH&zipcode=&measure=hospital-timely-and-effective-care
Medicare. (n.d.). Find healthcare providers: Compare care near you | Medicare. Medicare.gov. https://www.medicare.gov/care-compare/details/hospital/420004/view-all?city=Charleston&state=SC&zipcode=29425
Ong, B. N., Hodgson, D., Small, N., Nahar, P., & Sanders, C. (2020). Implementing a digital patient feedback system: An analysis using normalisation process theory. BioMed Central Health Services Research, 20(1), 387. https://doi.org/10.1186/s12913-020-05234-1
Osei, E., Asante, L. S., Wireko, S. A., & Abdulai, P. M. (2025). Digital health interventions for managing medication and healthcare service delivery by health professionals in Sub-Saharan Africa: A scoping review protocol. Digital Health, 11. https://doi.org/10.1177/20552076251379770
Pal, P., Sambhakar, S., Dave, V., Paliwal, S. K., Paliwal, S., Sharma, M., Kumar, A., & Dhama, N. (2021). A review of emerging smart technological innovations in healthcare sector for increasing patient’s medication adherence. Global Health Journal, 5(4), 183–189. https://doi.org/10.1016/j.glohj.2021.11.006
Provenzano, M., Cillara, N., Curcio, F., Pisu, M. O., Iván, C., & Herrera, M. F. J. (2024). Electronic health record adoption and its effects on healthcare staff: A qualitative study of well-being and workplace stress. International Journal of Environmental Research and Public Health, 21(11), e1430. https://doi.org/10.3390/ijerph21111430
Razick, D., Amani, N., Ali, L., Bachir, M., Salem, A., & Khatri, V. (2024). Leapfrog safety grades in California Hospitals: A data analysis. American Journal of Medical Quality, 39(5), 251–255. https://doi.org/10.1097/jmq.0000000000000200
Ricciardi, W., & Cascini, F. (2020). Guidelines and safety practices for improving patient safety.PubMed. Springer. https://www.ncbi.nlm.nih.gov/books/NBK585634/
The Leapfrog Group. (2023, November 3). New hospital safety grades from The Leapfrog Group find improved infection rates following a major spike during the COVID-19 pandemic. Leapfrog.org. https://www.leapfroggroup.org/news-events/new-hospital-safety-grades-leapfrog-group-find-improved-infection-rates-following-major
Appendix for
NURS FPX 8022 Assessment 1
Appendix A: Current Medication Communication and Discharge Workflow
Appendix B: Redesigned Workflow with Interactive Patient Education Systems and Automated Medication Dispensing
Capella Professors To Choose From For NURS-FPX8022 Class
- Jacqueline McCoy.
- Jessica Mioduszewski.
- Arezu Moussavi.
- Jennifer Naimark.
- Andrea Murray.
(FAQs) related to
NURS FPX 8022 Assessment 1
Question 1: Where can I download the complete assessment for NURS FPX 8022 Assessment 1?
Answer 1: You can download the complete NURS FPX 8022 Assessment 1 from tutorsacademy.co.
Question 2: What is NURS FPX 8022 Assessment 1 Using Data to Make Evidence-Based Technology Recommendations?
Answer 2: NURS FPX 8022 Assessment 1 involves making evidence-based technology recommendations in healthcare using data analysis.
Do you need a tutor to help with this paper for you within 24 hours
- 0% Plagiarised
- 0% AI
- Distinguish grades guarantee
- 24 hour delivery