NURS 8310 Week 10 Assignment FREE DOWNLOAD
NURS 8310 Week 10 Assignment
Program Proposal
Student Name
Walden University
NURS 8310 Epidemiology and Population Health
Professor Name
Date
Program Proposal to Address Heart Disease in African Americans
The Centers for Disease Control and Prevention (CDC, 2023) states that heart disease is the number one cause of death among adults in the United States, and it causes about 1 out of every 5 deaths, or approximately 695,000 deaths per year. African American adults have the highest cardiovascular-related mortality of all the racial and ethnic groups, with deaths about 30 percent more than the deaths of White Americans.
The contrast is especially high in southern states, including Georgia, where the geographic, economic, and access to healthcare factors combine to form compounded risks. Disproportionate systems and structural inequities put the African American adult population at a further disadvantage in rural Georgia, where heart disease is most prevalent (Fasehun et al., 2024).
Geographic Region and Population Characteristics
Georgia has many counties that are classified as Medically Underserved Areas (MUAs) by the Health Resources and Services Administration (HRSA) in its rural areas. These areas have also been characterized by profound challenges to proper healthcare provision, among them being the chronic scarcity of primary care physicians, inaccessibility to specialist care like cardiologists, and insufficiency in urgent care services.
Most of these regions have little or no public transportation infrastructure, and, as a result, getting to and from medical visits is particularly challenging when one does not have a car. Hospitals and clinics are also overwhelmed to the extent that patients have to travel more than 30 miles to get to the nearest hospital (Behr et al., 2022).
The rural Georgia African American population is socioeconomically deprived. The average unemployment rates in these communities are 8-10 percent, which is almost twice as much as the national percentage, and the median household income is less than 35,000 dollars a year, in comparison to a state median of more than 65,000 dollars in Georgia.
There is also a lack of educational attainment, as just a small percentage of African American adults in such regions have a college degree, serving to cause inadequate health literacy and difficulty in treating chronic diseases like hypertension and diabetes.
Patterns of Heart Disease Using Epidemiologic Characteristics
The epidemiological path of heart disease in the case study of the African American adults in rural Georgia is a complex interaction of biological, behavioral, and environmental factors. The rates of cardiovascular disease deaths in this population segment are the highest in the nation, and, in the rural counties, cardiovascular disease mortality is 15-25 percent higher in comparison with urban counties.
Men between 45 and 64 are especially at risk because of the late diagnosis, irregular adherence to treatment, and non-compliance with medications. Seasonal changes indicate an increase in emergency room visits and hospitalization in colder seasons, which can be connected to improper heating, psychological pressure, and the complications of comorbid respiratory diseases.
In addition, epidemiological patterns indicate that up to 25% of African American adults in rural Georgia have undiagnosed hypertension, and 50-60% of the affected patients are under control. Such statistics are worrying since hypertension is the only risk factor of heart disease that can be changed. On geographic maps, the rates of cardiovascular hospitalization are maximized in poor counties with large proportions of the African American population. Moreover, rural facilities usually do not have the ability to conduct more advanced cardiovascular procedures, and, as a result, patients must wait longer and achieve poorer results (Salehi et al., 2021).
Health Outcome to Improve
The main health outcome measure of this program includes the enhancement of blood pressure control among African American adults with uncontrolled Hypertension, which is a well-documented risk factor for heart disease, stroke, and kidney failure. The intervention will aim at decreasing the average values of systolic and diastolic blood pressure to the clinical target of <130/80 mmHg, consistent with the guidelines of the American Heart Association. Some of the core strategies will be to encourage regular intake of antihypertensive medicine, daily self-monitoring, and increased access to routine visits to the health facility (Nguyen-Huynh et al., 2022).
To facilitate these goals, the program will focus on behavioral change strategies, including goal setting, motivational interviewing, and peer support. Culturally appropriate instructional materials will be disseminated to assist participants in identifying the symptoms of high blood pressure, controlling the sodium content of the diet, and to learn the value of medication even in the absence of symptoms. The initiative will enable long-term health self-efficacy by encouraging active involvement of patients and trusting relationships between healthcare providers and the community. Finally, by decreasing the occurrence of hypertensive crises and emergency interventions, one will not only enhance patient outcomes but will also reduce healthcare expenditures and enhance the continuity of care in the region.
Current Evidence Supporting the Health Outcome
The validity of early and sustained hypertension management in preventing cardiovascular disease, such as heart attack, stroke, and heart failure, is always supported by scientific literature. A landmark SPRINT trial (2015) showed that the reduced systolic blood pressure of less than 120 mmHg, as compared to the standard blood pressure of 140 mmHg, substantially decreased the occurrence of heart attack, stroke, heart failure, and cardiovascular mortality by almost 25 percent. These results are of great concern, especially to high-risk demographics such as African American adults who have an earlier occurrence and worse outcomes of the complications surrounding hypertension. A report by the CDC further highlighted that African American populations derive more benefits from structured interventions aiming at medication adherence, dietary adaptation, and physical activity (Nguyen-Huynh et al., 2022).
In addition to clinical trials, there is real-world evidence that proves the efficacy of community-based interventions in the reduction of hypertension among underserved populations. These types of programs, like the Barbershop Hypertension Study, demonstrated that when trusted members of the community were involved in health education, there was considerable blood pressure control among African American males. Likewise, health monitoring apps and telemedicine systems have been successfully implemented in raising rural adherence and follow-up, where face-to-face visits are challenging.
Evidence-Based Program Approach
This program will take the form of a hybrid community clinic that will use Community Health Workers (CHWs), mobile clinics, and digital health technologies to provide education, monitoring, and support to African-American adults in rural Georgia. CHWs who will be recruited within the local community will conduct culturally adapted education programs on hypertension, nutrition, physical activity, and stress management. Such meetings will be conducted in local, trusted places like churches, community centers, and schools. All the participants will be provided with an authenticated home blood pressure measuring device and practical training on how to monitor themselves correctly.
Follow-ups through a mobile app, phone call, or text will be made weekly to monitor progress, troubleshoot obstacles, and motivate CHWs to engage on a regular basis. The model focuses on interprofessional relationships, whereby a routine coordination of CHWs, primary care providers, pharmacists, and behavioral health professionals is noted to enhance holistic, patient-centered care (Padalkar et al., 2024).
Besides these main elements, the program is made flexible and scalable, which is a major reason that it can be successful in rural environments. Mobile health clinics will take turns to visit underserved regions to give face-to-face evaluation, prescription refills, and in-person training to those with limited transport capacity. The remote involvement will be made possible by digital platforms that will send reminders, learning materials, and secure messaging with health teams. The printed materials and landline check-in will be offered to the participants who do not have smartphones or internet access (Ullah et al., 2023).
Data Collection and Analysis Plan
To evaluate the effectiveness and shape continuous improvement, the program will gather both quantitative and qualitative data to show results to stakeholders. Quantitative measures will be done through baseline and post-intervention blood pressure, rate of medication adherence, the number of clinic visits, as well as mobile unit visits and hospitalization rates due to cardiovascular complications. Accuracy will be obtained by using standardized tools, e.g., medication refill tracking and digital blood pressure logs. An attempt will be made to use pre- and post-intervention surveys to measure the increase in knowledge, satisfaction, and self-reported adherence (Belachew Bulo et al., 2024).
To supplement these measures, structured interviews and focus groups with participants, CHWs, and other stakeholders will be used to collect qualitative data. These discussions will cover the lived experiences of the participants, obstacles to participation, cultural understanding of hypertension, and recommendations for improvement of the program. The results of such discussions will assist in the enhancement of delivery techniques and cultural alignment. Analysis of the data will take the form of descriptive and inferential statistics to quantitative results with software like SPSS or R, and thematic coding of qualitative data to develop common trends and understandings at the community level (Ma et al., 2024).
SMART Objectives
The short-term goal of the program is to have a solid base of education and participation from the participants. At the end of the initial three months, at least 75 percent of participants will show a quantifiable improvement in the knowledge of hypertension, as assessed by using standardized pre- and post-intervention quizzes. Also, 60 percent of the participants will be able to attend at least three educational workshops in the first 90 days. These goals are aimed at enhancing awareness, encouraging health literacy, and establishing regular engagement, which are important aspects of behavior change when managing chronic disease (Choi et al., 2023).
In the case of long-term results, the program is aimed at providing long-term improvements in cardiovascular health. In 12 months, it is anticipated that 60 percent of the participants will be able to control blood pressure under 130/80 mmHg, which is in conformity with national clinical standards. In addition, the program is expected to lower the rate of readmission of patients with hypertensive complications by 20 percent in the intervention group, which implies effective management of the disease and a decrease in acute care consumption.
Stakeholders Involved in Planning
A wide range of stakeholders will be involved, through which the program will be community-driven, evidence-based, and sustainable. Local public health departments, regional hospitals, and Federally Qualified Health Centers (FQHCs) will be core collaborators and will offer clinical oversight, electronic health data access, and the ability to integrate with existing chronic disease initiatives. Local universities and community colleges will assist as academic centers of study, providing research assistance and student interns, as well as health education materials.
The partnerships with the pharmacy and nursing schools will allow students opportunities to receive experience in the form of clinical services and community engagement, and expand the program by using supervised clinical services. Such collaborations will also support the creation of a pipeline of culturally competent health practitioners who understand the issues related to rural health. Moreover, faith-based leaders, African American civic organizations, and community trusted individuals will be vital in establishing trust, improving recruitment, and directing culturally specific messages. A community advisory board inclusive of the healthcare professionals, past patients, caregivers, and local advocates, will give input in the development, implementation, and assessment of the program (Breeman et al., 2021).
Program Planning Model and Implementation Strategy
The Logic Model will be the guiding structure for the design, implementation, and evaluation of the program to handle it in a structured yet flexible way. The model has a clear picture of the necessary elements of the program. The inputs will be trained Community Health Workers (CHWs), mobile health vans, automated blood pressure monitors, culturally specific educational materials, grants, and administrative infrastructure. Such materials will facilitate various activities, including weekly educational programs, personalized home visits, phone or mobile application follow-ups, and community-based blood pressure screening programs.
Quantifiable measures of outputs will include the number of participants who are enrolled, the number of workshops conducted, the number of home visits, and the number of blood pressure readings. These will inform the short- and long-term results of the program, which will be aimed at raising the rates of hypertension control, enhancing the adherence to medications, and lowering the incidences of emergency room admissions associated with hypertensive crises.
The desired long-term effects are the measurable reduction of the prevalence of heart diseases in rural Georgia among the African American adult population and improved general quality of life. Adaptability is one of the key points of the model, where quarterly stakeholder evaluation meetings will be aimed at examining the trends in outcomes, getting feedback from the participants, and finding challenges in the implementation. The insights will guide the necessary changes at an appropriate time to keep the whole program culturally relevant, patient-centered, and community-sensitive (Coorey et al., 2021).
Cultural and Ethical Considerations
The use of cultural sensitivity will be one of the key principles in the design and delivery of the program. All program materials, such as brochures, videos, and content of the workshops, will also be culturally and linguistically adapted to the language, traditions, and values of the local African American community in rural Georgia. The training of Community Health Workers (CHWs) on implicit bias, cultural humility, and motivational interviewing will be completed to guarantee nonjudgmental, respectful interactions. Familiar community setting and relatable characters will be represented in visual aids, testimonials, and educational materials to create a sense of trust and relatability. To be language-accessible, interventions will be developed that use plain language and visual aids to reach people with low health literacy.
The program will be highly ethical in the sense that it will follow the rules of autonomy, transparency, and equity. Well-informed consent forms will be offered to all the participants, and the voluntary character of the program will be underlined throughout all the steps. People will have the freedom to opt out of the program at any time and not incur any penalty or loss of services. Strict confidentiality will be ensured, and the information will be anonymized and stored in a secure way and according to HIPAA requirements (Zhu et al., 2022).
Program Funding
The first source of funding for the program will be sought at the federal level, in such programs as the Health Resources and Services Administration (HRSA) Rural Health Care Services Outreach grants and the CDC Racial and Ethnic Approaches to Community Health (REACH) program. These sources of funding reflect the programmatic interest in reducing disparities in access to treatment of chronic disease in underserved populations and provide multi-year funding to implement and evaluate. Private health foundations, including the Robert Wood Johnson Foundation and Kaiser Permanente Community Health efforts, will also be tapped to obtain additional funding to support community involvement, workplace training, and health technology applications (Rajagopalan et al., 2024).
To meet the financial sustainability in the long run, the program will examine reimbursement of Community Health Worker (CHW) services through Medicaid State Plan Amendments or 1115 Waivers in coordination with the Georgia Department of Community Health. Covered services that are to be developed with billing strategies include health education, care coordination, or telemonitoring. The program team will also collaborate with managed care organizations and local insurers to integrate value-based care incentives that reimburse for better results of hypertension.
Marketing Strategies
The plan of marketing will focus on culturally sensitive, community-based outreach to fully leverage awareness, trust, and engagement of African American adults in rural Georgia. The campaign will be initiated by use of local institutions that are established and trusted in the community, such as church announcements, broadcasting on gospel radio stations, and by placing flyers in barbershops, beauty shops, and corner stores, which are usual community meeting points.
Community Health Workers (CHWs) will be essential in individual promotion because they will post testimonials and video stories through social media (Facebook, Instagram), which is widely used in rural communities. Community activities such as blood pressure monitoring days, demonstrations of healthy cooking, and physical challenges will generate exposure, attract walk-in visitors, and foster relationships with the locals.
To create an inclusive approach and maintain a long-term interaction, the proposed marketing plan will also feature a specially focused outreach to more difficult-to-reach audiences, including homebound elderly and people lacking access to the internet. Residents who are not inclined to digital communication will be reached through printed newsletters, robocalls, and bulletin boards in the community. The collaboration with the local African American fraternities, sororities, civic clubs, and health advocacy organizations will aid in extending the scope of the program and the assurance of credibility in the community (Bush et al., 2023).
Need help with NURS 8310 Week 4 Assignment Epidemiologic Study Designs? Click here for expert assistance.
Instructions To Write NURS 8310 Week 10 Assignment
Need instructions for this assessment? Contact us now and get expert guidance right away!
Instructions File For 8310 Week 10 Assignment
APPLYING EPIDEMIOLOGY TO PROGRAM DESIGN FOR CHRONIC DISEASE
Roughly 28.5 million Americans were still uninsured as of 2017, and 133 million Americans […] suffer from at least one chronic condition.
—Nash et al. (2021, p. 5)
As you know, promoting positive social change is a part of the Walden mission. To be an effective agent for social change, nurses must be able to logically and critically analyze population health issues using epidemiologic concepts, and then translate this knowledge into evidence-based practice to improve healthcare outcomes. This exercise will afford you such an experience at the population level. This is an exciting time to be working in the field of population health with all the new, dynamic, and innovative strategies to help patients and populations become more knowledgeable about their health.
Resources present numerous health problems that result in a need for ongoing care. Your ct a chronic disease of professional importance to you, and then design an intervention he health of populations affected by it.
TO PREPARE:
Review the Chronic Disease Prevention and Health Promotion (NCCDPHP) website from the Centers for Disease Control and Prevention (CDC).
Select one of the identified chronic diseases of national significance that impacts a population of interest to you.
Consider a health outcome you would like to improve in this population related to the selected chronic disease.
Develop a program proposal to improve this health outcome for this population using the assignment guidelines below. Select one of the program models in Curley, Chapter 8, to guide your planning.
Review the SMART objective resources for a review of how to write objectives for your program.
Use the Walden APA paper template, including appropriate APA 7 headings, to develop this Assignment.
THE ASSIGNMENT
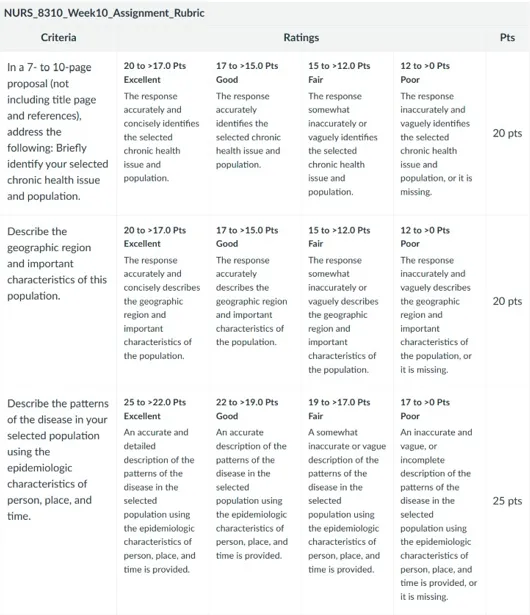
In a 7- to 10-page proposal (not including title page and references), address the following:
Briefly identify your selected chronic health issue and population.
Describe the geographic region and important characteristics of this population.
Describe the patterns of the disease in your selected population using the epidemiologic characteristics of person, place, and time.
Identify one health outcome you would like to improve for the population.
Briefly summarize current evidence that supports the importance of improving this health outcome.
Briefly describe the evidence-based program you are developing, and why this approach will best fit the needs of your population.
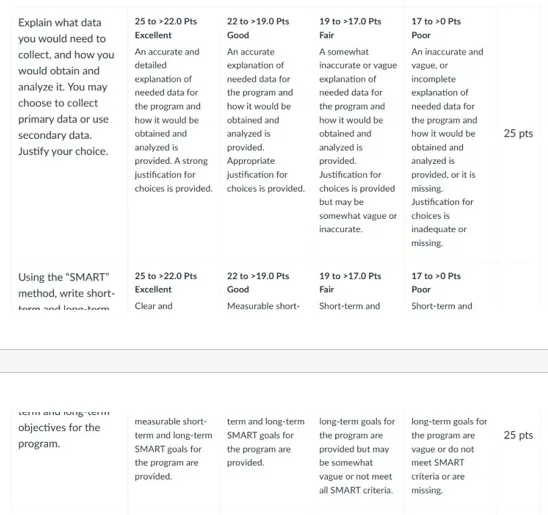
Explain what data you would need to collect, and how you would obtain and analyze it. You may choose to collect primary data or use secondary data. Justify your choice.
Using the “SMART” method, write short- and long-term objectives for the program.
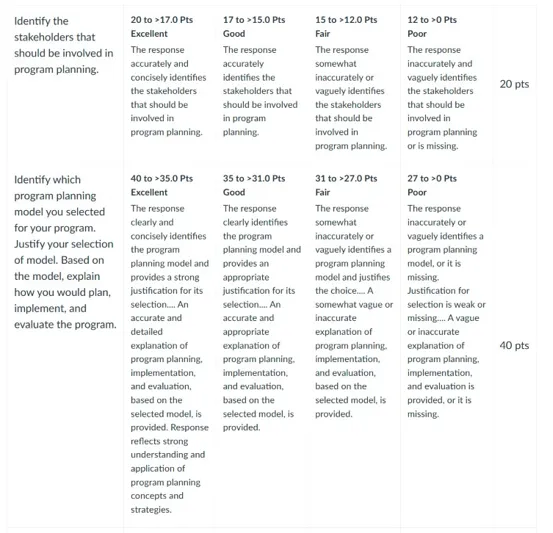
Identify the stakeholders who should be involved in program planning.
Identify which program planning model (see Curley, Chapter 7) you selected for your program. Justify your selection of model. Based on the model, explain how you would plan, implement, and evaluate the program.
Explain any relevant cultural or ethical considerations related to your program design.
Explain how you would fund the program.
Describe strategies that would be appropriate for marketing the program.
BY DAY 7 OF WEEK 10
Submit your Assignment.
SUBMISSION INFORMATION
Before submitting your final assignment, you can check your draft for authenticity. To check your draft, access the Turnitin Drafts from the Start Here area.
To submit your completed assignment, save your Assignment as WK10Assign_LastName_Firstinitial
Then, click on Start Assignment near the top of the page.
Next, click on Upload File and select Submit Assignment for review.
NURS 8310 Week 10 Assignment Rubrics



References For NURS 8310 Week 10 Assignment
Behr, C. L., Hull, P., Hsu, J., Newhouse, J. P., & Fung, V. (2022). Geographic access to federally qualified health centers before and after the Affordable Care Act. BMC Health Services Research, 22(1). https://doi.org/10.1186/s12913-022-07685-0
Belachew Bulo, Woldu, M., Beyene, A., Mekonnen, D., & Ephrem Engidawork. (2024). The impact of a medication therapy management service on the outcomes of hypertension treatment follow-up care in an Ethiopian tertiary hospital: A Pre-Post Interventional Study. Clinical Medicine Insights Cardiology, 18. https://doi.org/10.1177/11795468241274720
Breeman, L. D., Keesman, M., Atsma, D. E., Chavannes, N. H., Janssen, V., van Gemert-Pijnen, L., Kemps, H., Kraaij, W., Rauwers, F., Reijnders, T., Scholte op Reimer, W., Wentzel, J., Kraaijenhagen, R. A., & Evers, A. W. M. (2021). A multi-stakeholder approach to eHealth development: Promoting sustained healthy living among cardiovascular patients. International Journal of Medical Informatics, 147, 104364. https://doi.org/10.1016/j.ijmedinf.2020.104364
Bush, K., Patrick, C., Elliott, K., Morris, M., Tiruneh, Y., & McGaha, P. (2023). Unsung heroes in health education and promotion: How Community Health Workers contribute to hypertension management. Frontiers in Public Health, 11, 1088236. https://doi.org/10.3389/fpubh.2023.1088236
choi, e.-y., park, j.-s., min, d., ahn, s., & ahn, j.-a. (2023). heart failure-smart life: A randomized controlled trial of a mobile app for self-management in patients with heart failure. BMC Cardiovascular Disorders, 23(1). https://doi.org/10.1186/s12872-023-03039-8
Coorey, G., Peiris, D., Scaria, A., Mulley, J., Neubeck, L., Hafiz, N., & Redfern, J. (2021). An internet-based intervention for cardiovascular disease management integrated with primary care electronic health records: mixed methods evaluation of implementation fidelity and user engagement. Journal of Medical Internet Research, 23(4), e25333. https://doi.org/10.2196/25333
Fasehun, O. O., Adjei-Mensah, J., Ugorji, W. S., Titus, V. O., Asade, O. O., Adeyemo, D. A., & Okobi, O. E. (2024). Trends and patterns in hypertension-related deaths: A comprehensive analysis using the Centers for Disease Control and Prevention’s wide-ranging online data for epidemiologic research (CDC WONDER). Cureus. https://doi.org/10.7759/cureus.70754
Ma, L.-C., Lou, S.-N., Zhu, X.-L., Zhang, R.-L., Wu, L., Xu, J.-Y., Ding, X.-J., Liu, J., & Wang, Y. (2024). Needs and constraints for cardiac rehabilitation among patients with coronary heart disease within a community-based setting: A study based on focus group interviews. Patient Preference and Adherence, Volume 18, 1141–1150. https://doi.org/10.2147/ppa.s462138
Nguyen-Huynh, M. N., Young, J. D., Ovbiagele, B., Alexander, J. G., Alexeeff, S., Lee, C., Blick, N., Caan, B. J., Go, A. S., & Sidney, S. (2022). effect of lifestyle coaching or enhanced pharmacotherapy on blood pressure control among black adults with persistent uncontrolled hypertension: A cluster randomized clinical trial. JAMA Network Open, 5(5), e2212397. https://doi.org/10.1001/jamanetworkopen.2022.12397
Padalkar, T. V., Hildreth, K., Rocque, G. B., Ingram, S. A., Whitlow, O., Chu, D., Shao, C. C., Williams, C. P., Hardy, C. M., Huang, C.-H. S., & Henderson, N. L. (2024). Understanding multi-level factors impacting digital health literacy in the deep south of the United States. International Journal of Environmental Research and Public Health, 22(1), 41. https://doi.org/10.3390/ijerph22010041
Rajagopalan, N., Leung, S. W., Craft, R. S., & Bailey, A. L. (2024). improving cardiovascular health in the rural United States. JACC. Advances, 100950–100950. https://doi.org/10.1016/j.jacadv.2024.100950
Salehi, N., Janjani, P., Tadbiri, H., Rozbahani, M., & Jalilian, M. (2021). Effect of cigarette smoking on coronary arteries and pattern and severity of coronary artery disease: A review. The Journal of International Medical Research, 49(12). https://doi.org/10.1177/03000605211059893
Ullah, M., Hamayun, S., Wahab, A., Khan, S. U., Qayum, M., Ullah, A., Rehman, M. U., Mehreen, A., Awan, U. A., & Naeem, M. (2023). Smart technologies used as smart tools in the management of cardiovascular disease and their future perspective. Current Problems in Cardiology, 48(11), 101922. https://doi.org/10.1016/j.cpcardiol.2023.101922
Zhu, J. W., D’Angelo, F., Miranda, J. J., Yancy, C. W., Cupido, B., Zannad, F., & Van Spall, H. G. C. (2022). Incorporating cultural competence and cultural humility in cardiovascular clinical trials to increase diversity among participants. Journal of the American College of Cardiology, 80(1), 89–92. https://doi.org/10.1016/j.jacc.2022.05.001
Best Professors To Choose From For 8310 Class
- Julia Bucher
- Sue Bell
- Marilyn Losty
- Cara Krulewitch
- Cheryl Holly
(FAQs) related to NURS 8310 Week 10 Assignment
Question 1: Where can I download a free sample for NURS 8310 Week 10 Assignment?
Answer 1: You can download a free NURS 8310 Week 10 Assignment sample from Tutors Academy.
Question 2: Where can I find the rubrics and instructions for NURS 8310 Week 10 Assignment?
Answer 2: Detailed rubrics and instructions for NURS 8310 Week 10 Assignment are available at Tutors Academy.
Do you need a tutor to help with this paper for you with in 24 hours.
- 0% Plagiarised
- 0% AI
- Distinguish grades guarantee
- 24 hour delivery