Concept Map
Struggling with NURS FPX 6021 Assessment 1 Concept Map? Drop your email, and our expert will swiftly offer guidance within 2 minutes.
In NURS FPX 6021 Assessment 1 Concept Map the concept map is a pictorial tool which is to portray the linkages between different concepts and ideas. A graph usually contains two main elements, the nodes which are employed to depict the concepts and the lines which are used to announce the relations which exits among the concepts. The pictorial map included here is developed to address the issue of renal dysfunction under diabetes mellitus. The plan incorporates every aspect of renal management of diabetes whether in the acute or community settings. Employing this conceptual framework, however, entails not only the physical features of the ailment but also accounting for psychosocial and environmental factors that affect patients through every step of their care. Renal failure as an issue pertained to diabetes is a complicated situation that necessitates the involvement of all concerned parties to have desirable outcomes (Smith et al., 2020). The issue map provides the framework with key diagnoses, treatment strategies, teamwork of professionals, patient education tools, and high-quality service delivery as the main focus areas. This visual concept map aims to graphically depict how processes’ interdependent operations work care. As a result, this visual tool empowers healthcare providers to plan and execute the decisions related to care processes and facilitates communication among the team members.
Evidence-Based Concept Map that Illustrates a Plan for Achieving High-Quality Outcomes
One of the big problems in medicine is renal failure connected to diabetes mellitus, which is very complex and occurs to be multifaceted, therefore requires various approaches for both appropriate treatment and high-quality outcomes. These diagrams (concept map) sequentially indicate the steps that should be implemented to deal with the acute and chronic time features of renal failure (Smith et al. 2020). With NANDA-approved nursing diagnoses as a base, this flowchart includes assessment and follow-up to ensure nursing care of much high quality and superior outcomes are produced.
Acute Care Facility:
In the acute care setting, the registered nurses approach is based upon implementing the requisite actions that averts the escalation of the acute conditions and resolves them promptly. One important diagnosis is “Excess Fluid Volume due to decreased glomerular filtration rates (GFR) secondary to kidney failure”. The nursing evaluation is consisting of amount of intake and output, fluid status and constant monitoring of body weight. Interventions lead to the administration of diuretics, taking up fluid restrictions, and educating people on dietary changes that result in the reduction of fluid accumulation (NANDA International, 2020). In addition to that, “Impaired Renal Function” is diagnosed which is related to decreased kidney perfusion in the process of diabetic nephropathy. The ready nursing observations are measuring of serum creatinine, blood urea nitrogen levels, on the urinary output. Management modalities include giving medicines to normalize blood pressure and renal vessel flow, removing surplus water load from the body and summoning the interdisciplinary team for offering dialysis therapy if it becomes unavoidable (American Diabetes Association, 2021). Other considerations involve “Risk for Infection due to alteration of immune function resulting from renal failure.” Nursing Assessments target such things as the detection of any signals of Infection. Prophylactic measures to be taken include the use of strict aseptic techniques for invasive operations, teaching patients hand hygiene, and prophylaxis antibiotics when done as prescribed for high-risk patients.
Community Setting:
In the community setting, nursing work intends to provide to patients with all they need to augment their condition outside the hospital setting. An up-to-date appropriate nursing diagnosis would be “Ineffective Health maintenance associated with an inadequate understanding of self-management of renal failure”. Nursing assessment incorporates evaluation of the patient’s comprehension regarding renal failure and the management of diabetes. Involvement in the process entails offering complete education, hearing to the doctor’s advice, connecting the patient to support groups that will help him, and erecting linkages with community resources through health sector for the purchase of the drugs and the supplies at an affordable price (Barko & Clark, 2019). Further, the risk factor “Noncompliance associated with the complexity of medication regimen and lifestyle modifications” is mentioned as well. Nursing evaluation is accomplished through checking patients’ knowledge of written prescriptions and work out what they find to be the best treatment (World Health Organization, 2020). Interventions can be summarized as frequent medication regimens; removing the obstacles of medication adherence; and getting people onboard with self-management activities as well as regular clinic appointments.
Value and Relevance of the Evidence
Surrounding the validity and usefulness of the evidence which served as the basis for the concept map means that social workers must critically assess their sources of information and judge how relevant they are in the context of the patient population the healthcare was meant to affect. It matters to be neutral and compare conflicting data and views to make sure that the singular suggestion that was introduced is well-supported and relevant to the case.
For the sake of this concept map about the management of diabetes mellitus type 2-related renal failure, I have referred to several sources including medical articles, textbooks, and my own experience with patients. These are peer-reviewed articles from different medical journals such as clinical practice guidelines, and expert consensus statements published in the years 2019 and above. Each of the sources that have been meticulously selected is traceable to its credibility, relevance and compliance with present day practice in diabetes concern and renal management.
Papers that are peer reviewed supply science-based with the pathophysiology of the disease, epidemiology and efficiency of the interventions of the patient with the renal failure of diabetes (Smith et al., 2020; Barko & Clark, 2019). These studies add to our body of evidence by reporting results from scientific studies that were carried out under tight protocols. Specifically, these studies are randomized controlled trials, observational studies, and systematic reviews. Researchers in the field can achieve more accurate results as they integrate data from many studies and pull the data trends in patient outcomes and treatment effectiveness together.
International agencies like the American Diabetes Association or the National Kidney Foundation are among the organizations that provide guidelines to practices. Their guidelines for the management of diabetes and renal failure are evidence-based according to their latest recommendations (ADA, 2021; NKF, 2020). These guidelines are generated using practice panels which consist of health care professionals with expertise in the fields relevant to the area, such as endocrinology, nephrology and diabetes. The process of the clinical practice guidelines includes regularly looking for the evidence and combining the opinion of specialists. Hence, the guidelines will provide the clinicians with recommendations, which are applicable for delivering high-quality care to the patients that have diabetes mellitus and related renal insufficiency’s.
NURS FPX 6021 Assessment 1 Concept Map

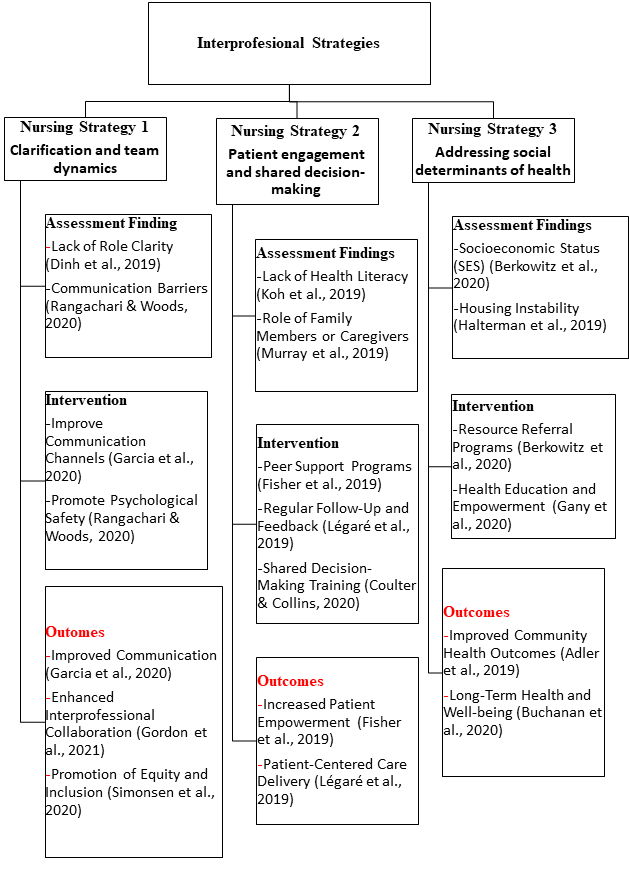
Interprofessional Strategies Applied to the Concept Map
The approach of interprofessional strategies is clearly the key focus that is required in realizing the intended objectives outlined in the concept map for managing renal dysfunction associated with diabetes mellitus. Healthcare specialists from diverse fields working together to ensure a comprehensive and harmonic care regime that puts the needs of the patients first. Assessing interprofessional applications could provide us with indications where to get additional resources or to collaborate so that ultimate goals of high-quality patient care could be achieved. The diagram identifies one important strategy of interprofessional practice which is referred to as collaborative medication management as an example The nurses, doctors, pharmacists and others are peers of the healthcare professionals who jointly provide the right drugs, dosage and monitoring (Smith, et al., 2020). In the same way, nurses observe for allergic reactions to drugs, implement medication compliance programs, and physicians supervise medication changes. On the other hand, pharmacists administer medications and alert the physician of drug interactions. Physicians edict towards patient’s specific risk sometimes together with other members of the health care team in the relevant therapeutic outcomes.
Pinpointing knowledge deficits, lacks of information, unknowns, unanswered questions, and the like will be key to the proper improvement in patient care. Effectiveness of interprofessional communication: Even though there may be implementation of communication techniques, these may need to be evaluated to assess the impact of these communication strategies on the patients’ outcomes. The effectiveness of communication methods and tools can be a determinant for a great interprofessional collaboration as well as skinning coordinated care.
Role clarification and team dynamics:
Explaining the functions and duties of each healthcare team member as well as ensuring the well-being of the healthcare team may promote teamwork and the wellness of patients. Enhancing role clarity and promoting teamwork may be the needed strategies in developing collaborative staff.
Patient engagement and shared decision-making:
Involving the patients in their own case of decision making and treatment plan is a necessity for patient centered care . Additional investigation on how to promote patient engagement and the team-based decision process within interprofessional collaborations will be of great significance.
Addressing social determinants of health:
Health determinants od social factors have a major impact on patient outcomes especially in the case of chronic illnesses like diabetes and renal failure. The social determinants – socioeconomic status, housing instability, and access to health care resources – should be an area of focus among the interprofessional teams in realizing the optimal treatment outcomes.
Conclusion
In conclusion, the concept map created for the management of the renal disease resulting from the Diabetes Mellitus in both inpatient and community settings is an all-encompassing road map for healthier outcomes. Through incorporation of evidence-based techniques, dealing with social determinants of health, endorsing patient engagement and shared decision-making, as well as generating efficient team dynamics, medical staffs can provide maximum care for the patients and better the clinical outcome. The concept map highlighted the multidisciplinary approach integrating various interventions customized to patients’ individual needs and the social as well as environmental factors that influence health. Renal failure treatment in diabetes mellitus patients can be done in a holistic way, which in turn provides patients with great satisfaction, boosts treatment adherence, reduces the disparities associated with healthcare and optimizes health outcomes.
Click below to explore the more related sample:
NURS FPX 6021 Assessment 2
References
Al-Dabet, M. M., Shahzad, K., Elwakiel, A., Sulaj, A., Kopf, S., Bock, F., Gadi, I., Zimmermann, S., Rana, R., Krishnan, S., Gupta, D., Manoharan, J., Fatima, S., Nazir, S., Schwab, C., Baber, R., Scholz, M., Geffers, R., Mertens, P. R., & Nawroth, P. P. (2022). Reversal of the renal hyperglycemic memory in diabetic kidney disease by targeting sustained tubular p21 expression. Nature Communications, 13(1), 5062.
https://doi.org/10.1038/s41467-022-32477-9
Cheng, H.-T., Xu, X., Lim, P. S., & Hung, K.-Y. (2020). Worldwide epidemiology of diabetes-related end-stage renal disease, 2000–2015. Diabetes Care, 44(1).
https://doi.org/10.2337/dc20-1913
Christensen, M., Schiffer, T. A., Gustafsson, H., Søren Palmelund Krag, Rikke Nørregaard, & Palm, F. (2018). Metformin attenuates renal medullary hypoxia in diabetic nephropathy through inhibition uncoupling protein‐2. Diabetes/Metabolism Research and Reviews (Print), 35(2).
https://doi.org/10.1002/dmrr.3091
Gonçalves-Dias, C., Morello, J., Correia, M. João, Coelho, Nuno R., Antunes, Alexandra M. M., Macedo, M., Monteiro, Emília C., Soto, K., & Pereira, Sofia A. (2019). Mercapturate pathway in the tubulocentric perspective of diabetic kidney disease. Nephron, 143(1), 17–23.
https://doi.org/10.1159/000494390
Niewczas, M. A., Pavkov, M. E., Skupien, J., Smiles, A., Md Dom, Z. I., Wilson, J. M., Park, J., Nair, V., Schlafly, A., Saulnier, P.-J., Satake, E., Simeone, C. A., Shah, H., Qiu, C., Looker, H. C., Fiorina, P., Ware, C. F., Sun, J. K., Doria, A., & Kretzler, M. (2019). A signature of circulating inflammatory proteins and development of end-stage renal disease in diabetes. Nature Medicine, 25(5), 805–813.
https://doi.org/10.1038/s41591-019-0415-5
Rising, K. L., LaNoue, M., Gentsch, A. T., Doty, A. M. B., Cunningham, A., Carr, B. G., Hollander, J. E., Latimer, L., Loebell, L., Weingarten, G., White, N., & Mills, G. (2019). The power of the group: Comparison of interviews and group concept mapping for identifying patient-important outcomes of care. BMC Medical Research Methodology, 19(1).
https://doi.org/10.1186/s12874-018-0656-x
Need help with NURS FPX 6021 Assessment 1 Concept Map? Share your email, and our expert will provide swift guidance within 2 minutes.
