NURS 6501 Week 3 Assignment FREE DOWNLOAD
NURS 6501 Week 3 Assignment
Cardiovascular Disorders
Student Name
Walden University
NURS 6501: Advanced Pathophysiology
Professor Name
Date
Concept Map Template
Primary Diagnosis: Aortic Aneurysm
Describe the pathophysiology of the primary diagnosis in your own words. What are the patient’s risk factors for this diagnosis?
Pathophysiology of Primary Diagnosis | |
Aortic aneurysm develops because structural deterioration within the arterial wall makes a specific area of the aorta weaken and expand (Gao et al., 2023). Progressive vessel dilation occurs due to sustained vessel stress which results in weakening of the material structure. The main cause of aortic aneurysm occurs through the deterioration of smooth muscle and elastic fibers found in the middle layer of the vessel wall called the tunica media. The arterial wall subjected to lipid and plaque accumulation in atherosclerosis develops inflammatory responses which diminishes the structural proteins elastin and collagen. When elasticity decreases in the aortic wall it becomes more likely for the vessel to expand when the body experiences blood pressure. Progressive aneurysm growth leads to the thinning of the vessel wall which raises the danger of either vessel rupture or dissection. | |
Causes | Risk Factors (genetic/ethnic/physical) |
| Genetic Risk Factors
Ethnic Risk Factors
Physical Risk Factors
|
What are the patient’s signs and symptoms for this diagnosis? How does the diagnosis impact other body systems and what are the possible complications?
Signs and Symptoms – Common presentation | How does the diagnosis impact each body system? Complications? |
|
|
What are other potential diagnosis that present in a similar way to this diagnosis (differentials)?
|
What diagnostic tests or labs would you order to rule out the differentials for this patient or confirm the primary diagnosis?
|
What treatment options would you consider? Include possible referrals and medications.
Medical Management The treatment plan for small aneurysms that show no symptoms includes only surveillance for both male patients and female patients with diameter measurements below 5.5 cm for men and 5.0 cm for women. Blood pressure control stands as the most important treatment approach which may involve daily beta-blocker doses at 50-100 mg of metoprolol combined with daily ACE inhibitor doses ranging from 10 to 40 mg of lisinopril to lower aortic wall tension (Gao et al., 2023). Patients should take atorvastatin at 40-80 mg daily dose to treat atherosclerosis and prevent damage to vessels. Patients must stop smoking while controlling their cholesterol levels as physicians must perform CT or ultrasound examinations every 6-12 months to track aneurysm enlargement. Surgical Intervention Medical teams should plan aortic surgery when aneurysm sizes reach 5.5 cm or big growth (>0.5 cm within 6 months) happens or if it causes symptoms that affect health. Surgical treatment of the affected area requires completely replacing the damaged section with synthetic material. Endovascular Aneurysm Repair (EVAR) is a less invasive procedure using a stent graft to reinforce the aorta and is preferred in high-risk surgical patients. Emergency surgery is required for ruptured aneurysms (Aljabri et al., 2024). Referrals A vascular surgeon or cardiothoracic surgeon needs to conduct surgical evaluations. Healthcare professionals from the cardiology specialty should evaluate blood pressure and lipid levels with patients. Patients requiring genetic assessment of potential causes need doctors specializing in hereditary issues. Consultations with pulmonologists or gastroenterologists must occur in cases where aortic aneurysms compress respiratory or digestive organs leading to complications. Lifestyle Modifications & Follow-Up The patient needs to follow a low-sodium heart-healthy diet while performing low-impact exercise and abstaining from heavy lifting to protect their aortic wall from strain. The treatment requires frequent imaging checks through ultrasound or CT scans as well as regular medicine dose adjustments. The treatment requires that patients receive education regarding how to detect aortic aneurysm rupture signs which include severe immediate pain along with dizziness and low blood pressure. |
Need help with your NURS 6501 Week 2 Assignment Case Study Analysis? Get expert guidance now!
Instructions To Write NURS 6501 Week 3 Assignment
Need instructions for this assessment? Contact us now and get expert guidance right away!
Instructions File For 6501 Week 3 Assignment
CARDIOVASCULAR DISORDERS
In this exercise, you will complete a MindMap to gauge your understanding of this week’s content. Select one of the possible topics provided to complete your MindMap.
myocardial infarction
congenital heart disease (may select ASD, VSD, or PDA)
peripheral arterial disease
peripheral vascular disease
valvular heart disease
cardiomyopathy (may select dilated, hypertrophic, or restricted)
atherosclerosis
aortic aneurysm
deep vein thrombosis
hypertension
heart failure
RESOURCES
Be sure to review the Learning Resources before completing this activity. Click the weekly resources link to access the resources.
WEEKLY RESOURCES
BY DAY 7 OF WEEK 3
Submit your MindMap by Day 7 of Week 3.
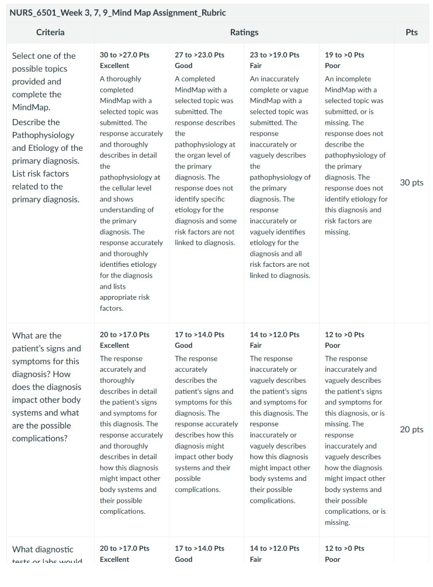
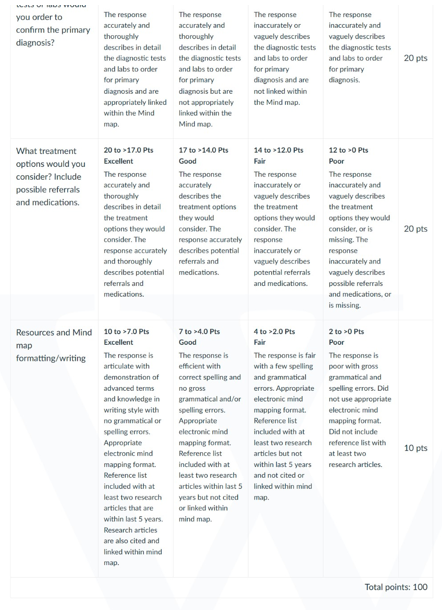
NURS 6501 Week 3 Assignment Rubrics
References For NURS 6501 Week 3 Assignment
Accarino, G., Giordano, A. N., Falcone, M., Celano, A., Vassallo, M. G., Fornino, G., Bracale, U. M., Vecchione, C., & Galasso, G. (2022). Abdominal aortic aneurysm: Natural history, pathophysiology and translational perspectives. Translational Medicine @ UniSa, 24(2), 30–40. https://doi.org/10.37825/2239-9747.1037
Aljabri, B., Iqbal, K., Alanezi, T., Al-Salman, M., Altuwaijri, T., Aldossary, M. Y., Alarify, G. A., Alhadlaq, L. S., Alhamlan, S. A., AlSheikh, S., & Altoijry, A. (2024). Thoracic endovascular aortic repair and endovascular aneurysm repair approaches for managing aortic pathologies: A retrospective cohort study. Journal of Clinical Medicine, 13(18), 5450. https://doi.org/10.3390/jcm13185450
Barbato, F., Allocca, R., Bosso, G., & Numis, F. G. (2022). Anatomy of cerebral arteries with clinical aspects in patients with ischemic stroke. Anatomia, 1(2), 152–169. https://doi.org/10.3390/anatomia1020016
Gao, J., Cao, H., Hu, G., Wu, Y., Xu, Y., Cui, H., Lu, H. S., & Zheng, L. (2023). The mechanism and therapy of aortic aneurysms. Signal Transduction and Targeted Therapy, 8(1), 1–20. https://doi.org/10.1038/s41392-023-01325-7
Ghazinour, M., Ghaedi, A., Bazrgar, A., Montaseri, M., Sasannia, M., & Drissi, H. B. (2024). A huge coronary artery aneurysm with ST-elevation myocardial infarction: A case report and review of literature. Heliyon, 10(19). https://doi.org/10.1016/j.heliyon.2024.e38511
Harjola, V., Parissis, J., Bauersachs, J., Brunner‐La Rocca, H., Bueno, H., Čelutkienė, J., Chioncel, O., Coats, A. J. S., Collins, S. P., Boer, R. A., Filippatos, G., Gayat, E., Hill, L., Laine, M., Lassus, J., Lommi, J., Masip, J., Mebazaa, A., Metra, M., & Miró, Ò. (2020). Acute coronary syndromes and acute heart failure: a diagnostic dilemma and high‐risk combination. A statement from the Acute Heart Failure Committee of the Heart Failure Association of the European Society of Cardiology. European Journal of Heart Failure, 22(8). https://doi.org/10.1002/ejhf.1831
Ion, A., Stafie, C., Mitu, O., Ciobanu, C. E., Halitchi, D. I., Costache, A. D., Bobric, C., Troase, R., Mitu, I., Huzum, B., Duca, S. T., & Costache, I. I. (2021). Biomarkers utility: At the borderline between cardiology and neurology. Journal of Cardiovascular Development and Disease, 8(11), 139. https://doi.org/10.3390/jcdd8110139
Narula, J., Chandrashekhar, Y., Ahmadi, A., Abbara, S., Berman, D. S., Blankstein, R., Leipsic, J., Newby, D., Nicol, E. D., Nieman, K., Shaw, L., Villines, T. C., Williams, M., & Hecht, H. S. (2021). SCCT 2021 expert consensus document on coronary computed tomographic angiography: A report of the society of cardiovascular computed tomography. Journal of Cardiovascular Computed Tomography, 15(3), 192–217. https://doi.org/10.1016/j.jcct.2020.11.001
Peypoch, O., Paüls-Vergés, F., Vázquez-Santiago, M., Dilme, J., Romero, J., Giner, J., Plaza, V., Escudero, J. R., Soria, J. M., Camacho, M., & Sabater-Lleal, M. (2020). The TAGA study: A study of factors determining aortic diameter in families at high risk of abdominal aortic aneurysm reveal two new candidate genes. Journal of Clinical Medicine, 9(4), 1242. https://doi.org/10.3390/jcm9041242
Soto, M. E., Ochoa-Hein, E., Anaya-Ayala, J. E., Ayala-Picazo, M., & Koretzky, S. G. (2021). Systematic review and meta-analysis of aortic valve-sparing surgery versus replacement surgery in ascending aortic aneurysms and dissection in patients with Marfan syndrome and other genetic connective tissue disorders. Journal of Thoracic Disease, 13(8), 4830–4844. https://doi.org/10.21037/jtd-21-789
Yuan, Z., Lu, Y., Wei, J., Wu, J., Yang, J., & Cai, Z. (2021). Abdominal aortic aneurysm: Roles of inflammatory cells. Frontiers in Immunology, 11. https://doi.org/10.3389/fimmu.2020.609161
Zeigler, S., Sloan, B., & Jones, J. A. (2021). The pathophysiology and pathogenesis of Marfan syndrome. Advances in Experimental Medicine and Biology, 1348, 185–206. https://doi.org/10.1007/978-3-030-80614-9_8
Best Professors To Choose From For NURS 6501 Class
- Dr. Mary Smith
- Dr. Tara Harris
- Dr. Mahaman Moussa
- Dr. Annaliza (Anna Liza) Villena
- Dr. Morgan Skinner
(FAQs) related to NURS 6501 Week 3 Assignment
Question 1: Where can I download a free sample for NURS 6501 Week 3 Assignment?
Answer 1: Download a free sample from Tutors Academy.
Question 2: Where can I find the rubrics and instruction file for NURS 6501 Week 3 Assignment?
Answer 2: Get the rubric and instruction file from the Tutors Academy website.
Do you need a tutor to help with this paper for you with in 24 hours.
- 0% Plagiarised
- 0% AI
- Distinguish grades guarantee
- 24 hour delivery