- NURS FPX 8030 Assessment 2 Evidenced-Based Literature Search and Organization.
Evidence-Based Literature Search and Organization
Staffing needs have been around for as long as anyone can study in the clinical benefits field. Short staffing can be a beast of stress for patient safety. Patient safety can be affected by the higher speed of patient falls, Cauti’s, Hapi’s, and lower patient satisfaction scores. Inadequate staffing influences patient care and can cause nursing staff to eliminate errands due to nonappearance of time. There is a need to search for overseas staffing issues for this basic test in clinical benefits that influence clinical orderlies. Explore our assessment NURS FPX 8030 Assessment 1 for more information.
This paper aims to search for evidence of the believability of adequate staffing ratios and whether it can energize patient satisfaction scores within one year. The following is the PICOT question:
How do safe staffing ratios of 1:6 compared to unsafe staffing ratios of less than 1:6 affect patient safety in hospital patients?
P – Clinical educated authorities
I – Safe staffing ratios 1:6
C – Unsafe staffing ratios less than 1:6
O – Patient satisfaction scores and diminishing of patient safety issues. T – a half year
Search for Literature
The main stage in the NURS FPX 8030 Assessment 2 Evidence-Based Literature Search and Organization process is distinguishing an issue that influences clinical guards. I distinguished staffing ratios and how they influence clinical regulators and patients constantly. Then, a PICOT question was formulated that distinguishes everybody, which for this ongoing circumstance is the Clinical guardians. Then, the watchwords are handily seen, which fans out a blueprint for a framework for searching. Watchwords are an essential part of the informational collection search.
The following stage is finished, identifying the information bases that would be searched. In requesting research, various sources are searched for material and reliable information. For instance, the fundamental watchwords that were used in the search included clinical regulators, nursing ratios, patient satisfaction, patient safety, and a half year. This step also includes the ID of search engines to be utilized. The search engines used were CINAHL Finished and Nursing and Collaborated Wellbeing.
- Literature Search Process
A general search was conducted using both truncation and Boolean connectors. Truncation searched for nurse*, which pulled up clinical regulators and nursing. Boolean connector AND was used with patient safety and patient satisfaction, which searched for patient topics that included safety and satisfaction.
The following stage to be tended to is ensuring that the inclusion/avoidance models are considered while identifying the meaning of the articles searched for. One inclusion was that the articles were to be peer-investigated articles. The articles were additionally not to be more settled than five years; all articles picked were not more settled than 2019, andmost were within three years. This date range gave current, pertinent information for the topic picked.
NURS FPX 8030 Assessment 2 Evidenced-Based Literature Search and Organization
All articles were open as full text and online, which obliged straightforwardness and accessibility when researching the topic. In the literature search, five gigantic articles were picked that fit the research topic. Dismissal standards included articles that were more prepared than five years, articles that were not peer-assessed, and articles that did not include patients in a hospital setting. Banished equivalently showed restraint masses where the patients were determined to have precious wellbeing issues, mental suspension, or dementia. These patient social classes were confined from the search since getting wary information and examination from these patient masses is vexatious.
Research Articles
The articles picked were according to the following:
1. Exploring the relationship among showed and saw the commitment of clinical bosses and related work demands, work resources, and individual resources; a longitudinal report (Van Sanctum Oetelaar et al., 2021).
2. Impact of Double Intensive Thought Unit and Fast Response Gathering Nursing Position on Help Advancement in the Intensive Thought Unit (Fildes et al., 2022).
3. Rethinking Nursing Effectiveness: An Overview of the Literature and Interviews with Thought Trailblazers (Disch & Finis, 2022).
4. What Do Orderlies Need to Practice in the Hospital Environment? An Integrative Review With Considerations for Clinical Coordinated Trailblazers (Kowalski et al., 2020).
5. An Outline of Missed Nursing Care and Its Predictors in Saudi Arabia: A Cross-Sectional Survey (Al Muharraq et al., 2022).
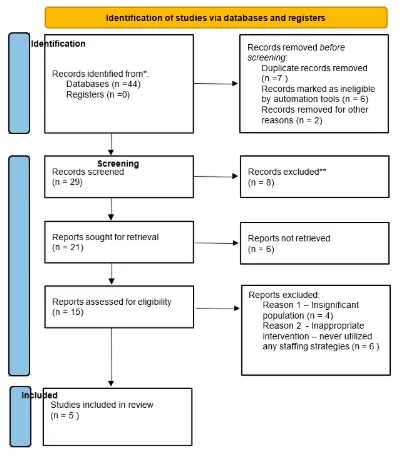
PRISMA Chart Analysis
The articles above were picked since they fulfilled the inclusion gauges and discussed nursing staffing ratios and patient satisfaction. They all contain information that has been late within the last five years. All articles are peer-surveyed and are substantial information. A PRISMA chart was utilized in the ID of concentrates through informational varieties and registers, see Reference section 1. A PRISMA outline assembles the records accumulated from the informational indexes searched and gives a stream sheet reflecting articles eliminated, recuperated, qualified, denied, and included in the study (Page et al., 2020).
A PRISMA chart is an essential tool in NURS FPX 8030 Assessment 2 Evidence-Based Literature Search and Organization, as it visually represents the number of studies identified, screened, and included based on inclusion criteria. It helps track records eliminated before the screening, denied after the screening, and retrieved for further review, ensuring a structured and systematic approach to organizing evidence-based research.
References
Al Muharaaq, E. H., Alallah, S., M., Alkhayrat, S. A., & Jahlan, A. G. (2022). An overview of missed nursing care and its predictors in Saudi Arabia: A cross-sectional study. Nursing Research and Practice, 2022. https://doi.org/10.1155/2022/4971890
Disch, J., & Finis, N. (2022). Rethinking nursing productivity: A literature review and interviews with thought leaders. Nursing Economics, 40(2), 59-71.
Fildes, C., Munt, R., & Chamberlain, D. (2022). Impact of dual intensive care unit and rapid response team nursing roles on service delivery in the intensive care unit. Critical Care Nurse, 42(5), 23–31. https://doi.org/10.4037/ccn2022540
Kowalski, M. O., Basile, C., Bersick, E., Cole, D. A., McClure, D. E., & Weaver, S. H. (2020). What do nurses need to practice effectively in the hospital environment? An integrative review with implications for nurse leaders. Worldviews on Evidence-Based Nursing, 17(1), 60–70. https://doi.org/10.1111/wvn.12401
McHugh, M. D., Aiken, L., H., S., D. M., W., C., D., C., & Yates, P. (2021).
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffman, T. C., Mulrow, C. D., et al. The PRISMA 2020 statement is an updated guideline for reporting systemic reviews. BMJ, 2021. https://doi.org/10.1136/bmj.n71
Wilhelmina, F. J. M. van den, Oetelaar, Roelen, C. A. M., Grolman, W., Stellato, R. K., & Willem, v. R. (2021). Exploring the relation between modeled and perceived workload of nurses and related job demands, job resources and personal resources; a longitudinal study. PLoS One, 16(2). https://doi.org/10.1371/journal.pone.0246658
Appendix 1
PRISMADiagram