NURS 6052 Module 3 Assignment FREE DOWNLOAD
NURS 6052 Module 3 Assignment
Evidence-Based Project, Part 2: Advanced Levels of Inquiry and Systemic Reviews
Student Name
NURS6052
Walden University
Professor Name
Date
Slide 1:
The focus of the presentation Medication administration errors (MAEs) through a systematic review of literature in order to focus on non-punitive reporting systems and educational interventions as potential solutions.
Slide 2:
Objectives
Examine medication administration errors
Analyze non-punitive solutions
Evaluate educational interventions
Apply PICO(T) framework
Improve medication safety
Medication administration errors (MAEs) are a critical patient safety element in nursing practice, typically due to system failure, inadequate training, or retaliatory reporting environments. The evidence-based project explores MAEs through systematic literature review, with emphasis on the non-punitive reporting systems and educational interventions as feasible alternatives. Using the PICO(T) strategy, it critically appraises peer-reviewed articles from databases like PubMed, CINAHL, Scopus, and Web of Science to determine feasible error-reduction strategies. Through analysis of high-level evidence, the appraisal demonstrates how organizational change and education for nurses are effective ways of improving medication safety within acute care.
Slide 3:
Clinical Issue
Medication administration error (MAE)
Key issue in patient safety and nursing practice
Medication administration: core of nursing
Clinical Issue of Interest: Medication Administration Errors in Nursing Practice
Medication administration error (MAE) is a key issue in patient safety and nursing practice. These errors occur where there is a divergence from the planned medication regimen, e.g., wrong drug, wrong dosage, inappropriate route, or incorrect timing. MAEs have important patient outcomes such as length of stay in hospital, healthcare costs, and patient harm and even death (Jessurun et al., 2022). The major implications involved, the knowledge of the underlying causes, reporting barriers, and minimizing these errors via interventions to improve the quality of clinical care. Medication administration lies at the core of nursing; therefore, nurses are key stakeholders that must be engaged in addressing this issue.
The incidence of MAEs has been widely reported in a wide range of settings across the world. Research has been carried out by Tariq et al. (2024), which has identified some of the reasons including communication breakdowns, suboptimal training, interruptions during medication rounds, and system breakdowns as critical among the main reasons behind such errors. Additionally, underreporting of MAEs continues to be a problem due to fear of blame, legal repercussions, or disciplinary action. Solution to this complex issue necessitates systemic intervention by way of education, redesign of the system, and establishment of safety and transparency culture. Hence, identification of evidence-based practices to reduce MAEs is imperative in terms of improving nursing practice and patient wellbeing.
Slide 4:
PICO(T) Question
In registered nurses working in acute care hospitals (P), how does the implementation of non-punitive error reporting systems and targeted educational programs (I), compared to current punitive error management practices and limited educational support (C), affect medication administration error rates and nurse compliance with reporting protocols (O) over a 6–12 month period (T)?
Development of the PICO(T) Question
To structure my clinical inquiry around medication administration errors, I formulated a PICO(T) question that focuses on the intervention of interest, its impact, and the context in which it applies. The acronym PICO(T) stands for Population, Intervention, Comparison, Outcome, and Timeframe. In this case:
Population (P): Registered nurses working in acute care hospitals.
Intervention (I): Implementation of non-punitive error reporting systems and targeted educational programs.
Comparison (C): Current practices involving punitive error management and limited educational support.
Outcome (O): Reduction in medication administration errors and improved nurse compliance with error reporting protocols.
Timeframe (T): Over a period of 6–12 months following implementation.
The PICO(T) question was developed following a critical review of the literature and consideration of gaps in existing practice. By focusing on interventions like non-punitive reporting and education, my aim is to study methods that not only reduce errors but also encourage an active safety culture in nurses. My PICO(T) question will form the crux of my evidence-based project and guide my search for relevant studies and systematic reviews during the course.
Slide 5:
Research Databases
PubMed biomedical focus
CINAHL nursing specialty
Scopus interdisciplinary coverage
Web of Science citations
Comprehensive evidence base
Research Databases Used for Literature Search
To perform a careful and extensive search for peer-reviewed journal articles on medication administration mistakes, I searched four main databases offered by the Walden Library: PubMed, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Scopus, and Web of Science. These databases offer individual advantages and links to wide sets of scholarly resources relevant to nursing and healthcare studies. PubMed, administered by the U.S. National Library of Medicine, is a valuable resource for biomedical literature (Jin et al., 2024). The database contains millions of citations for MEDLINE, life science journals, and electronic books, and hence is appropriate for identifying high-quality studies on medication safety, nursing practices, and patient outcomes. Its sophisticated filters for searching allow identification of systematic reviews, meta-analyses, and other filtered evidence types required to answer clinical questions with the highest level of scientific precision.
CINAHL is tailored specifically for nursing and allied health professionals, with access to a big database of nursing literature, conference proceedings, and evidence-based care sheets. Since the aim of this project was nursing practice and the administration of drugs, CINAHL provided targeted literature directly addressing the clinical issue at hand. Its robust indexing system facilitates precise searching with controlled vocabulary terms such as CINAHL Headings, enhancing the quality and the relevance of retrieved articles.
Scopus is a vast abstract and citation database of peer-reviewed literature, encompassing all the major disciplines like health sciences, social sciences, and humanities. Scopus excels in cross-disciplinary research and offers tracking, analysis, and visualization features for research trends (Baas et al., 2020). Scopus’s extensive coverage supports identifying landmark and path-breaking research on medication error and prevention measures. Finally, Web of Science provides multidisciplinary coverage and robust citation mapping capabilities, which allow authors to track how ideas evolve over a period of time and determine seminal studies in a field. Powerful Boolean searching and availability of high-impact journals are provided by this database, which prove useful when searching for systematic reviews and meta-analyses that aggregate results from many different studies. With the use of these databases, I presented a systematic and thorough method of looking for the best existing evidence about medication administration errors within nursing practice.
Slide 6:
Systematic Reviews (1/2)
Afaya, A., Konlan, K. D., & Kim Do, H. (2021). Improving patient safety through identifying barriers to reporting medication administration errors among nurses: An integrative review. BMC Health Services Research, 21(1), 1–10. https://doi.org/10.1186/s12913-021-07187-5
Brabcová, I., Hajduchová, H., Tóthová, V., Chloubová, I., Červený, M., Prokešová, R., Malý, J., Vlček, J., Doseděl, M., Malá-Ládová, K., Tesař, O., & O’Hara, S. (2023). Reasons for medication administration errors, barriers to reporting them and the number of reported medication administration errors from the perspective of nurses: A cross-sectional survey. Nurse Education in Practice, 70(1), 103642. https://doi.org/10.1016/j.nepr.2023.103642
Slide 7:
Systematic Reviews and High-Level Evidence Articles Identified
Using keywords from my PICO(T) question, i.e., medication administration error, nursing, non-punitive reporting, education, and systematic review, I was successful to identify four peer-reviewed articles on the meta-analysis or systematic review level. The four articles provide high-level evidence addressing various issues of medication administration errors, i.e., causes, reporting barriers, and potential interventions.
Afaya, A., Konlan, K. D., & Kim Do, H. (2021). Improving patient safety through identifying barriers to reporting medication administration errors among nurses: An integrative review. BMC Health Services Research, 21(1), 1–10. https://doi.org/10.1186/s12913-021-07187-5
The integrative review integrates evidence from a number of studies to examine organizational and individual barriers that discourage nurses from reporting medication errors. Authors cite fear of retaliation, lack of confidentiality, and poor institutional policies as key barriers to reporting. This review is most closely analogous to the comparison component of my PICO(T) question, that is, existing punitive vs. non-punitive systems.
Brabcová, I., Hajduchová, H., Tóthová, V., Chloubová, I., Červený, M., Prokešová, R., Malý, J., Vlček, J., Doseděl, M., Malá-Ládová, K., Tesař, O., & O’Hara, S. (2023). Reasons for medication administration errors, barriers to reporting them and the number of reported medication administration errors from the perspective of nurses: A cross-sectional survey. Nurse Education in Practice, 70(1), 103642. https://doi.org/10.1016/j.nepr.2023.103642
Although the paper is a cross-sectional study rather than a systematic review, it is high-level quantitative data that explores both the reason for MAEs and reluctance to report them. The extremely large sample size (n=1,205) and standardized survey instrument provide it with good validity and reliability. It deals with the intervention element of the PICO(T) question by emphasizing the need for improved training and supportive cultures to reduce errors.
Slide 8:
Systematic Reviews (2/2)
Fathy, A. S. M., Khalil, N. S., Abd-elbaky, M. M., & Taha, N. (2020). Nurse’s knowledge and practice regarding medication errors in critical care units: Descriptive study. Minia Scientific Nursing Journal, 008(1), 111–120. https://doi.org/10.21608/msnj.2020.188051
Tsegaye, D., Alem, G., Tessema, Z., & Alebachew, W. (2020). Medication administration errors and associated factors among nurses. International Journal of General Medicine, 13(13), 1621–1632. https://doi.org/10.2147/ijgm.s289452
Fathy, A. S. M., Khalil, N. S., Abd-elbaky, M. M., & Taha, N. (2020). Nurse’s knowledge and practice regarding medication errors in critical care units: Descriptive study. Minia Scientific Nursing Journal, 008(1), 111–120. https://doi.org/10.21608/msnj.2020.188051
This is descriptive research evaluating the knowledge and current practices of nurses on medication errors in critical care settings. It illustrates significant knowledge deficits and inconsistent practice, especially among recent graduates. Although the design is descriptive, the results support the necessity for targeted education, an intervention central to my PICO(T) question.
Tsegaye, D., Alem, G., Tessema, Z., & Alebachew, W. (2020). Medication administration errors and associated factors among nurses. International Journal of General Medicine, 13(13), 1621–1632. https://doi.org/10.2147/ijgm.s289452
Cross-sectional study of prevalence and risk factors for MAEs in Ethiopian referral centers identifies common causes such as inadequate training, heavy workload, and interruptions during medication rounds. This is not a systematic review but employs effective primary data to address the population and outcome aspects of the PICO(T) question.
Slide 9:
Levels of Evidence and Strengths of Systematic Reviews
Afaya et al. (2021) is an integrative review (Level I)
Other Three are Cross-sectional studies (Level III)
Large sample strengths
Standardized instruments
Statistical validity
Levels of Evidence and Strengths of Systematic Reviews
Of the four articles examined, Afaya et al. (2021) is an integrative review (Level I evidence) and three others are descriptive or cross-sectional studies (Level III evidence). Although there are no meta-analyses among the selected articles, collectively, they present solid empirical evidence for the nature, etiology, and solution to medication administration errors in nursing practice. Systematic reviews, like the integrative review of Afaya et al. (2021), are the most superior form of evidence (Level I) since they use strict methods to synthesize data from numerous studies in a thorough manner. Systematic reviews reduce bias via preselected inclusion/exclusion criteria, quality appraisal of included studies, and explicit data synthesis methods. For example, Afaya et al. utilized the Mixed Methods Appraisal Tool (MMAT) to evaluate the quality of studies included in order to only utilize high-quality evidence to inform their conclusions. The strength of systematic reviews is that they can provide an overview of the literature overall, distinguish patterns, and offer recommendations based on cumulative evidence rather than isolated findings.
Cross-sectional studies, which are lower in the hierarchy of evidence, still have valid contributions, especially if conducted on large samples and using validated instruments. Brabcová et al. (2023) are an excellent case in that they conducted a survey of over 1,200 nurses using a validated instrument. That they used statistical techniques such as Pearson correlation and CHAID analysis lends support to the internal validity of their findings. Similarly, Tsegaye et al. (2020) used binary logistic regression to identify independent predictors of MAEs to make more robust generalizations about causal associations.
Slide 10:
Conclusion
Punitive culture harms
Education reduces errors
System redesign needed
Higher evidence required
Safety culture imperative
Findings of the systematic review support that medication administration errors continue to occur despite punitive reporting cultures, lack of knowledge, and workflow system problems in the system. Although integrative reviews and cross-sectional studies yield helpful information regarding the causes and interventions for MAE, more senior evidence is required to define best practice. The study emphasizes the importance of the implementation of non-punitive reporting systems along with targeted education interventions to enhance medication safety, thus ensuring improved patient outcomes and openness of nursing practice.
Explore the full NURS 6052 Module 2 Assignment Evidence-Based Project guide and get expert-written samples now!
Instructions To Write NURS 6052 Module 3 Assignment
Need instructions for this assessment? Contact us now and get expert guidance right away!
Instructions File For 6052 Module 3 Assignment
EVIDENCE-BASED PROJECT, PART 2: ADVANCED LEVELS OF CLINICAL INQUIRY AND SYSTEMATIC REVIEWS
Your quest to purchase a new car begins with an identification of the factors important to you. As you conduct a search of cars that rate high on those factors, you collect evidence and try to understand the extent of that evidence. A report that suggests a certain make and model of automobile has high mileage is encouraging. But who produced that report? How valid is it? How was the data collected, and what was the sample size?
In this Assignment, you will delve deeper into clinical inquiry by closely examining your PICO(T) question. You also begin to analyze the evidence you have collected.
RESOURCES
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
WEEKLY RESOURCES
To Prepare:
Review the Resources and identify a clinical issue of interest that can form the basis of a clinical inquiry.
Develop a PICO(T) question to address the clinical issue of interest you identified in Module 2 for the Assignment. This PICO(T) question will remain the same for the entire course.
Use the keywords from the PICO(T) question you developed and search at least four different databases in the Walden Library. Identify at least four relevant systematic reviews or other filtered high-level evidence, which includes meta-analyses, critically-appraised topics (evidence syntheses), critically-appraised individual articles (article synopses). The evidence will not necessarily address all the elements of your PICO(T) question, so select the most important concepts to search and find the best evidence available.
Reflect on the process of creating a PICO(T) question and searching for peer-reviewed research.
The Assignment (Evidence-Based Project)
Part 2: Advanced Levels of Clinical Inquiry and Systematic Reviews
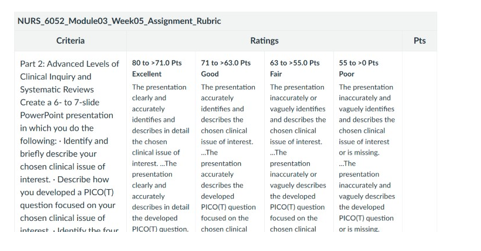
Create a 6 to 7-slide PowerPoint presentation in which you do the following:
Identify and briefly describe your chosen clinical issue of interest.
Describe how you developed a PICO(T) question focused on your chosen clinical issue of interest.
Identify the four research databases that you used to conduct your search for the peer-reviewed articles you selected.
Provide APA citations of the four relevant peer-reviewed articles at the systematic-reviews level related to your research question. If there are no systematic-review level articles or meta-analysis on your topic, then use the highest level of evidence peer-reviewed article.
Describe the levels of evidence in each of the four peer-reviewed articles you selected, including an explanation of the strengths of using systematic reviews for clinical research. Be specific and provide examples.
BY DAY 7 OF WEEK 5
Submit Part 2 of your Evidence-Based Project.
SUBMISSION INFORMATION
Before submitting your final assignment, you can check your draft for authenticity. To check your draft, access the Turnitin Drafts from the Start Here area.
To submit your completed assignment, save your Assignment as MD3Assgn+last name+first initial
Then, click on Start Assignment near the top of the page.
Next, click on Upload File and select Submit Assignment for review.
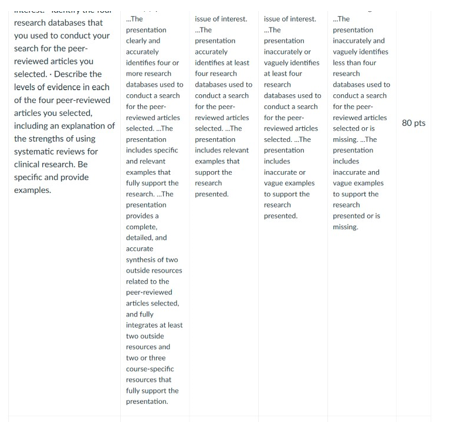
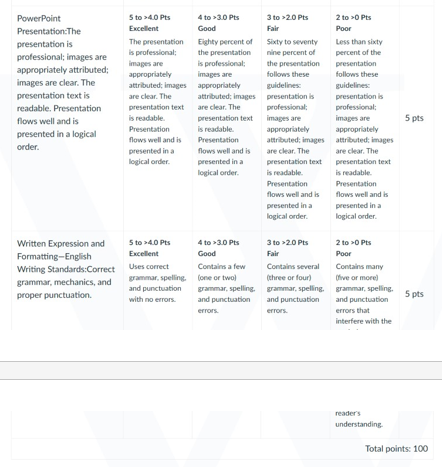
NURS 6052 Module 3 Assignment Rubrics
References For NURS 6052 Module 3 Assignment
Afaya, A., Konlan, K. D., & Kim Do, H. (2021). Improving patient safety through identifying barriers to reporting medication administration errors among nurses: An integrative review. BMC Health Services Research, 21(1), 1–10. https://doi.org/10.1186/s12913-021-07187-5
Baas, J., Schotten, M., Plume, A., Côté, G., & Karimi, R. (2020). Scopus as a curated, high-quality bibliometric data source for academic research in quantitative science studies. Quantitative Science Studies, 1(1), 377–386. https://doi.org/10.1162/qss_a_00019
Brabcová, I., Hajduchová, H., Tóthová, V., Chloubová, I., Červený, M., Prokešová, R., Malý, J., Vlček, J., Doseděl, M., Malá-Ládová, K., Tesař, O., & O’Hara, S. (2023). Reasons for medication administration errors, barriers to reporting them and the number of reported medication administration errors from the perspective of nurses: A cross-sectional survey. Nurse Education in Practice, 70(1), 103642. https://doi.org/10.1016/j.nepr.2023.103642
Fathy, A. S. M., Khalil, N. S., Abd-elbaky, M. M., & Taha, N. (2020). Nurse’s knowledge and practice regarding medication errors in critical care units: Descriptive study. Minia Scientific Nursing Journal, 008(1), 111–120. https://doi.org/10.21608/msnj.2020.188051
Jessurun, J. G., Hunfeld, N. G. M., Roo, M., Onzenoort, H. A. W., Rosmalen, J., Dijk, M., & Bemt, P. M. L. A. (2022). Prevalence and determinants of medication administration errors in clinical wards: A two‐centre prospective observational study. Journal of Clinical Nursing, 32(1-2), 208–220. https://doi.org/10.1111/jocn.16215
Jin, Q., Leaman, R., & Lu, Z. (2024). PubMed and beyond: Biomedical literature search in the age of artificial intelligence. EBioMedicine, 100(26), 104988–104988. https://doi.org/10.1016/j.ebiom.2024.104988
Tariq, R., Scherbak, Y., Vashisht, R., & Sinha, A. (2024, February 12). Medication dispensing errors and prevention. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK519065/
Tsegaye, D., Alem, G., Tessema, Z., & Alebachew, W. (2020). Medication administration errors and associated factors among nurses. International Journal of General Medicine, 13(13), 1621–1632. https://doi.org/10.2147/ijgm.s289452
Best Professors To Choose From For NURS 6052 Class
- Dr. Donna Hathorn
- Dr. Judith (Judy) Cornelius
- Dr. Danielle Beasley
- Dr. Usama Saleh
- Dr. Wendy Ostendorf
(FAQs) related to NURS 6052 Module 3 Assignment
Question 1: Where can I download a free sample for NURS 6052 Module 3 Assignment?
Answer 1: Download a free sample from Tutors Academy.
Question 2: Where can I find the rubrics and instruction file for NURS 6052 Module 3 Assignment?
Answer 2: Get the rubric and instruction file from the Tutors Academy website.
Do you need a tutor to help with this paper for you with in 24 hours.
- 0% Plagiarised
- 0% AI
- Distinguish grades guarantee
- 24 hour delivery