NURS 6052 Module 4 Assignment FREE DOWNLOAD
NURS 6052 Module 4 Assignment
Evidence-Based Project, Part 3: Critical Appraisal of Research
Student Name
Walden University
NURS 6052: Essentials of Evidence-Based Practice
Professor Name
Date
Evaluation Table
Medication Administration Error in Nursing Practice
Use this document to complete the evaluation table requirement of the Module 4 Assessment, Evidence-Based Project, Part 3A: Critical Appraisal of Research
Full APA-formatted citation of selected article. | Article #1 | Article #2 | Article #3 | Article #4 |
Afaya, A., Konlan, K. D., & Kim Do, H. (2021). Improving patient safety through identifying barriers to reporting medication administration errors among nurses: An integrative review. BMC Health Services Research, 21(1), 1–10. https://doi.org/10.1186/s12913-021-07187-5 | Bell, T., Sprajcer, M., Flenady, T., & Sahay, A. (2023). Fatigue in nurses and medication administration errors: A scoping review. Journal of Clinical Nursing, 32(17-18), 5445–5460. Wiley Online Library. https://doi.org/10.1111/jocn.16620 | Alrabadi, N., Shawagfeh, S., Haddad, R., Mukattash, T., Abuhammad, S., Al-rabadi, D., Abu Farha, R., AlRabadi, S., & Al-Faouri, I. (2021). Medication errors: a focus on nursing practice. Journal of Pharmaceutical Health Services Research, 12(1), 78–86. https://doi.org/10.1093/jphsr/rmaa025 | D’Errico, S. (2022). Medication Errors in Pediatrics: Proposals to improve the quality and safety of care through clinical risk management. Frontiers in Medicine, 8(814100). https://doi.org/10.3389/fmed.2021.814100 | |
Evidence Level * (I, II, or III) | Level III This is an integrative review that combines both qualitative and quantitative non-experimental studies, which falls under Level III per the Johns Hopkins model. | Level III This is a scoping review, which involves synthesizing non-experimental studies. According to the Johns Hopkins Evidence-Based Practice Model, this qualifies as Level III evidence. | Level V This article is a narrative literature review, primarily based on existing publications found via PubMed and Google Scholar. It does not involve primary research or a systematic methodology, and therefore falls under Level V in the Johns Hopkins Evidence-Based Practice Model. | Level V The article is a narrative literature review, based on existing studies retrieved via PubMed and manual searching. It does not present original research or use a systematic/meta-analytic methodology, which places it in Level V according to the Johns Hopkins Nursing Evidence-Based Practice model. |
Conceptual Framework Describe the theoretical basis for the study (If there is not one mentioned in the article, say that here).** | None stated The abstract does not specify a theoretical or conceptual framework guiding the review. It focuses on identifying barriers without grounding them in a specific theory. | None explicitly mentioned The study does not describe a theoretical framework. It is guided by Arksey and O’Malley’s scoping review framework and uses the PAGER framework for data analysis, but no theoretical model for fatigue or errors is applied. | None stated The article does not present a theoretical or conceptual framework. It is a general review aimed at increasing awareness of medication errors, particularly by nurses. | None stated The review does not explicitly state a theoretical or conceptual framework. It is focused on risk profiling and clinical strategies rather than being guided by a specific model. |
Design/Method Describe the design and how the study was carried out (In detail, including inclusion/exclusion criteria). | Integrative Review
| Scoping Review
| Narrative Literature Review
| Narrative Literature Review
P (Patient): Pediatric patients I (Intervention): Drug therapy O (Outcome): Adverse events/medication errors
Epidemiology Care setting (hospital/outpatient) Risk factors Adverse events Personalization of therapy |
Sample/Setting The number and characteristics of patients, attrition rate, etc. | Total articles retrieved: 10,929 Final studies included: 14 Characteristics: All studies focused on nurses in the hospital setting Attrition rate: Not applicable (literature review, not a primary study on patients) | Number of studies included: 38 Population studied: Registered nurses in hospital settings No specific patient or attrition details provided (since it’s a review) | Not applicable (This is not a primary research study) No sample of participants or settings is included The general focus is on clinical practice involving nurses |
|
Major Variables Studied List and define dependent and independent variables |
| Independent variables:
Dependent variables:
| No specific variables are defined or measured However, the review discusses:
| No statistical variables were measured in this paper The main themes discussed include:
|
Measurement Identify primary statistics used to answer clinical questions (You need to list the actual tests done). | Primary evaluation method: Qualitative synthesis and thematic analysis Quality assessment tool: MMAT 2018 Specific statistical tests are not mentioned, as it is an integrative review that synthesizes data from various designs | No uniform method of measurement due to heterogeneity across studies Tools and metrics used in included studies varied (fatigue measures were inconsistent) Not a meta-analysis; no specific statistical tests reported | No statistical measurements or tools were used The article does not perform quantitative or qualitative analysis It functions as a broad overview based on available literature |
7.5 million preventable medication errors annually in U.S. pediatric patients 14–31% of pediatric medication errors result in harm or death Pediatric patients account for 31% of all reported medication errors versus 13% in adults (USP report) |
Data Analysis, Statistical or Qualitative findings (You need to enter the actual numbers determined by the statistical tests or qualitative data.) |
Organizational barriers:
Professional/individual barriers:
| Key finding:
Fatigue outcomes:
Contributing factors:
Inconsistency noted in measurement methods and findings among studies | No numerical data or statistical tests were reported Key qualitative insights include:
| No original statistical analysis performed Key statistics cited from other sources:
The article integrates epidemiological data and thematic risk profiles to present a high-level analysis |
Findings and Recommendations General findings and recommendations of the research | Findings:
Recommendations:
| Findings:
Recommendations:
| Findings:
Recommendations:
| Findings:
Dosage adjustment needs Off-label drug use Formulation and measurement complexity Communication and documentation issues Recommendations:
Protocol adherence Documentation accuracy Communication improvement Staff education and strategic planning |
Appraisal and Study Quality Describe the general worth of this research to practice. What are the strengths and limitations of the study? What are the risks associated with the implementation of the suggested practices or processes detailed in the research? What is the feasibility of use in your practice? | Strengths:
Limitations:
Risks of Implementation:
Feasibility:
| Strengths:
Limitations:
Risks of Implementation:
Feasibility:
| Strengths:
Limitations:
Risks of Implementation:
Feasibility:
| Strengths:
Limitations:
Risks of Implementation:
Feasibility:
|
Key findings | The main barriers to reporting medication administration errors are:
| Fatigue is a major contributor to medication errors due to:
82% of studies confirmed this relationship There is no standardized approach to measuring fatigue in healthcare literature | Nurses are essential to error prevention MEs have severe physical, psychological, and economic consequences Reporting and preventive strategies (standardized processes, training, communication) are crucial Emphasis on creating blame-free and supportive environments in hospitals | Pediatric medication errors are more frequent and more harmful than in adults Primary risks: dose miscalculations, off-label use, formulation changes High-risk settings: Emergency Departments, NICUs, and ICUs Preventive strategies must include:
|
Outcomes | Emphasizes the need for:
| Fatigue negatively impacts patient safety via impaired nursing performance
|
| Improved safety through understanding and targeting pediatric-specific risks Better governance and error management through structured protocols and training Support for international alignment on pediatric medication safety practices Encouragement of further research and data transparency |
General Notes/Comments |
Critical Appraisal of Research
Medication administration errors (MAEs) are a serious risk to patient safety and particularly in hospitals where nurses are the last point of safety in medication administration. One of the key points that appeared in the reviewed literature consistently is the fact that underreporting of such errors is caused not only by system-level factors but also by individual ones. According to the evaluation of the four identified studies, one of the best practices of promoting patient safety and minimizing MAEs is the creation of a non-punitive, supportive reporting climate.
According to Afaya, Konlan, and Kim Do (2021), fear of punishment, ignorance, and ambiguous definitions were found to be the major hindrances to error reporting. Their integrative review highlighted that nurses tend to fail to report errors because of a blame culture and the lack of organizational support. One of the key recommendations made by their study is to adopt non-punitive policies and educational programs that would encourage error transparency and learning (Afaya et al., 2021).
Bell et al. (2023) also touched upon the systemic factors that contribute to MAEs, with special attention to nurse fatigue that was associated with reduced vigilance and more errors in more than 80 percent of the studies considered. Although fatigue is an independent problem that needs to be addressed with staffing and scheduling changes, the root cause behind both mistakes and error reporting still exists: when errors are made under fatigue, nurses will be less likely to report the error because of possible retribution, particularly in high-stress areas.
Alrabadi et al. (2021) also advocate the necessity of systemic changes that rely on education, open dialogue, and reporting and error prevention guideline clarity. Even though the review is not systematic, it confirms that the establishment of a blame-free culture allows nurses to report errors without fear, thus making root cause analysis and institutional learning possible.
Lastly, D Errico (2022) emphasized the susceptibility of pediatric patients to medication errors and the need to have strong governance systems, training, and standard documentation. The paper highlighted the importance of open communication and clinical risk management, which can only be possible in a setting where employees are psychologically secure to report and discuss mistakes without the fear of being punished.
Collectively, evidence is overwhelming to the use of non-punitive reporting culture as a best practice. This strategy includes the explicit definition of MAEs, the safeguarding of the staff against disciplinary penalties in case of reporting accidental mistakes, and the incorporation of supportive education and leadership training. By creating such a culture, accountability and ongoing improvement are encouraged instead of blame, and eventually, patient outcomes are improved.
Explore the full NURS 6052 Module 3 Assignment Evidence-Based Project guide and download expert-written samples now!
Instructions To Write NURS 6052 Module 4 Assignment
Need instructions for this assessment? Contact us now and get expert guidance right away!
Instructions File For 6052 Module 4 Assignment
EVIDENCE-BASED PROJECT, PART 3: CRITICAL APPRAISAL OF RESEARCH
Realtors rely on detailed property appraisals—conducted using appraisal tools—to assign market values to houses and other properties. These values are then presented to buyers and sellers to set prices and initiate offers.
Research appraisal is not that different. The critical appraisal process utilizes formal appraisal tools to assess the results of research to determine value to the context at hand. Evidence-based practitioners often present these findings to make the case for specific courses of action.
In this Assignment, you will use an appraisal tool to conduct a critical appraisal of published research. You will then present the results of your efforts.
RESOURCES
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
To Prepare:
Reflect on the four peer-reviewed articles you selected in Module 2 and the four systematic reviews (or other filtered high-level evidence) you selected in Module 3.
Reflect on the four peer-reviewed articles you selected in Module 2 and analyzed in Module 3.
Review and download the Critical Appraisal Tool Worksheet Template provided in the Resources.
The Assignment (Evidence-Based Project)
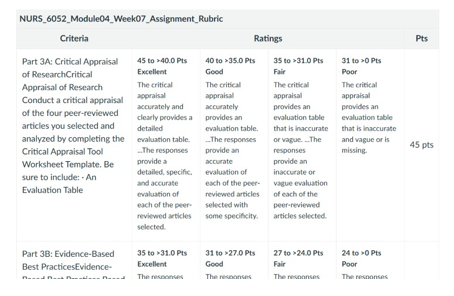
Part 3A: Critical Appraisal of Research
Conduct a critical appraisal of the four peer-reviewed articles you selected by completing the Evaluation Table within the Critical Appraisal Tool Worksheet Template. Choose a total of four peer-reviewed articles that you selected related to your clinical topic of interest in Module 2 and Module 3.
Note: You can choose any combination of articles from Modules 2 and 3 for your Critical Appraisal. For example, you may choose two unfiltered research articles from Module 2 and two filtered research articles (systematic reviews) from Module 3 or one article from Module 2 and three articles from Module 3. You can choose any combination of articles from the prior Module Assignments as long as both modules and types of studies are represented.
Part 3B: Critical Appraisal of Research
Based on your appraisal, in a 1-2-page critical appraisal, suggest a best practice that emerges from the research you reviewed. Briefly explain the best practice, justifying your proposal with APA citations of the research.
BY DAY 7 OF WEEK 7
Submit Part 3A and 3B of your Evidence-Based Project.
SUBMISSION INFORMATION
Before submitting your final assignment, you can check your draft for authenticity. To check your draft, access the Turnitin Drafts from the Start Here area.
To submit your completed assignment, save your Assignment as MD4Assgn+last name+first initial.
Then, click on Start Assignment near the top of the page.
Next, click on Upload File and select Submit Assignment for review.
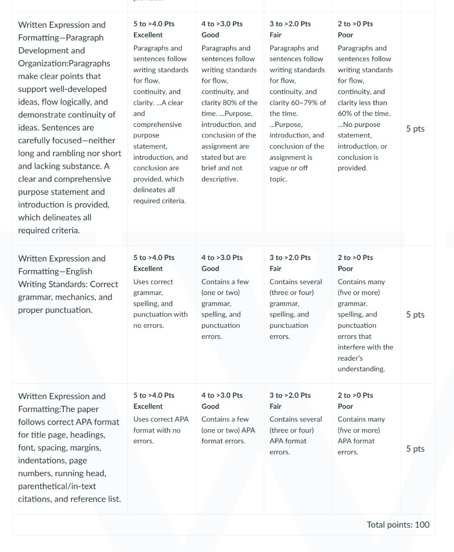
NURS 6052 Module 4 Assignment Rubrics

References For NURS 6052 Module 4 Assignment
Afaya, A., Konlan, K. D., & Kim Do, H. (2021). Improving patient safety through identifying barriers to reporting medication administration errors among nurses: An integrative review. BMC Health Services Research, 21(1), 1–10. https://doi.org/10.1186/s12913-021-07187-5
Bell, T., Sprajcer, M., Flenady, T., & Sahay, A. (2023). Fatigue in nurses and medication administration errors: A scoping review. Journal of Clinical Nursing, 32(17-18), 5445–5460. Wiley Online Library. https://doi.org/10.1111/jocn.16620
Alrabadi, N., Shawagfeh, S., Haddad, R., Mukattash, T., Abuhammad, S., Al-rabadi, D., Abu Farha, R., AlRabadi, S., & Al-Faouri, I. (2021). Medication errors: A focus on nursing practice. Journal of Pharmaceutical Health Services Research, 12(1), 78–86. https://doi.org/10.1093/jphsr/rmaa025
D’Errico, S. (2022). Medication errors in pediatrics: Proposals to improve the quality and safety of care through clinical risk management. Frontiers in Medicine, 8(814100). https://doi.org/10.3389/fmed.2021.814100
Best Professors To Choose From For NURS 6052 Class
- Dr. Donna Hathorn
- Dr. Judith (Judy) Cornelius
- Dr. Danielle Beasley
- Dr. Usama Saleh
- Dr. Wendy Ostendorf
(FAQs) related to NURS 6052 Module 4 Assignment
Question 1: Where can I download a free sample for NURS 6052 Module 4 Assignment?
Answer 1: Download a free sample from Tutors Academy.
Question 2: Where can I find the rubrics and instruction file for NURS 6052 Module 4 Assignment?
Answer 2: Get the rubric and instruction file from the Tutors Academy website.
Do you need a tutor to help with this paper for you with in 24 hours.
- 0% Plagiarised
- 0% AI
- Distinguish grades guarantee
- 24 hour delivery