NURS FPX 6424 Assessment 3 Sample FREE DOWNLOAD
NURS FPX 6424 Assessment 3 Proposal to Administration: Spreadsheet and Video Presentation
Student Name
Capella University
NURS-FPX6424 Data Mining to Advance Healthcare
Professor Name
Submission Date
Proposal to Administration: Spreadsheet and Video Presentation
Good day, honorable administrators. I am ________. Welcome to this spreadsheet and video presentation. The purpose in the present day would be to convey conclusions and recommendations regarding the 30-day hospital readmission rate among heart failure patients, which would be selected as the purpose, because of its direct association with the effectiveness of care coordination.
Evidence shows that high readmission rates due to gaps in discharge planning, suboptimal follow-up, or inadequate patient self-management are standard (Macchio et al., 2020). By combining the Iowa Model with health informatics tools such as Electronic Health Records (EHRs), predictive analytics, and clinical decision support systems, it is possible to identify at-risk patients early, personalize interventions, and ultimately reduce readmissions.
Analyzing What, why, and how to measure a Specific Quality Outcome
To analyze why patients with heart failure return within 30 days, we examine medication adherence, follow-up frequency, patient satisfaction, and weight change. The “What” is the readmission rate and secondary indicators, which are reviewed monthly to assess how the situation is changing and identify opportunities for improvement.
The purpose of this is to support care coordination, reduce hospital readmissions, and align with CMS expectations (Anawade et al., 2024). For “How,” information is gathered from electronic medical records, data analysis is performed to identify risks, and patient surveys and medication use logs are used. Using all these methods, we can fully track patients’ progress, enabling us to make data-driven choices for long-term gains.
First, the primary outcome under analysis is the 30-day readmission rate of heart failure patients. This indicator is a benchmark endorsed by the Centers for Medicare & Medicaid Services (CMS), which has a target rate below 20 percent (Macchio et al., 2020). Achieving or exceeding this benchmark means that care teams have successfully addressed transitional care gaps.
Alongside readmission rates, secondary benchmarks include medication adherence, follow-up appointment attendance, patient satisfaction, and average weight gain, which are correlated with successful chronic disease management (Baryakova et al., 2023). These benchmarks are measured monthly to enable timely course corrections. Regular measurement also ensures compliance with national performance standards and supports data-driven decision-making.
Data collection methods have been carefully selected to target both clinical and behavioural contributors to readmission. EHR extraction is the process of obtaining objective clinical data, such as discharge dates, readmission occurrences, and other documented symptoms, such as weight gain or dyspnea. Predictive analytics algorithms then analyze this data to identify a group of patients who exhibit patterns indicating a risk of developing the problem, including sudden weight gain of 2 pounds in 24 hours.
Pharmacy refill records and patient-reported adherence data are used to calculate medication adherence, and outpatient scheduling logs are used to calculate follow-up attendance rates. Patient satisfaction surveys, conducted with validated tools such as the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), provide a window into engagement and perceived quality of care (Cui et al., 2025). Collecting these data every month enables trend analysis and early intervention, and is in keeping with the Iowa Model’s emphasis on evidence-based practice and collaboration with stakeholders.
Analyzing Quality Outcome Data Trends
Data evaluation concerns measuring and tracking month-to-month changes in the metrics against established benchmarks. For example, the readmission rate fell from 22% in January to 16% in June, representing a relative improvement of 6%. This trend is associated with increased medication adherence (70% to 85%) and follow-up rates (55% to 75%) over the same period. Pham et al. showed that a 10% increase in the percentage of days covered (PDC) by cardiovascular medications was associated with a 6% decrease in hospital admissions.
In addition, patient satisfaction increased from 65% to 78%, indicating greater engagement and a higher perceived quality of care. The average weight had decreased from 5.2 pounds to 3.5 pounds over six months, an important early warning sign of fluid buildup in heart failure.
By identifying weight gain “red flags”, nonadherence, and missed appointments using real-time EHR queries, nurses and pharmacists could monitor and intervene and adjust diuretics, reinforce education, or establish a telephonic follow-up visit. Sutton et al. (2020) showed that clinical decision support built into EHRs can facilitate these workflows, thereby reducing fragmented care processes.
In fact, when the service line rolled out an EHR-led notification system in March, the Patient Satisfaction score increased by 25%, and readmissions decreased by 18% by June. These interconnected improvements provide robust evidence that informatics-driven enhancements, in combination with the Iowa Model, are fueling meaningful quality improvements.
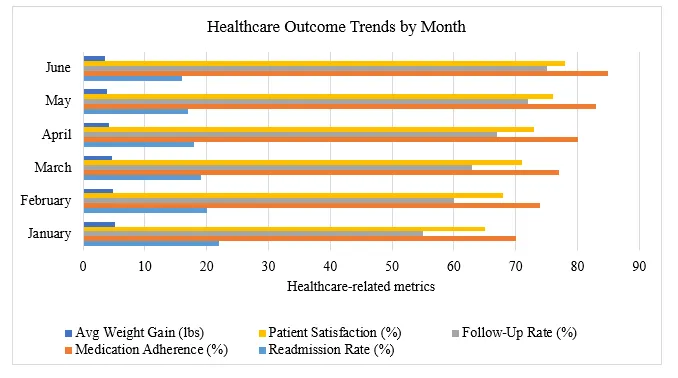
Looking into the details of the spreadsheet, the rows represent the months of the calendar year, from January to June, and the columns give the readmission rate (%), the medication adherence (%), the follow-up rate (%), the patient satisfaction (%), and the average weight gain (lbs.) (see Table 1).
It can be seen from the above that as adherence increased, from 70% in January to 85% in June, the rate of readmission decreased. This alignment helps emphasize the cause-and-effect relationship between the patient’s behavior and clinical outcomes.
Table 1: Healthcare Outcome Trends by Month
Month | Readmission Rate (%) | Medication Adherence (%) | Follow-Up Rate (%) | Patient Satisfaction (%) | Avg Weight Gain (lbs) |
January | 22 | 70 | 55 | 65 | 5.2 |
February | 20 | 74 | 60 | 68 | 4.9 |
March | 19 | 77 | 63 | 71 | 4.6 |
April | 18 | 80 | 67 | 73 | 4.2 |
May | 17 | 83 | 72 | 76 | 3.9 |
June | 16 | 85 | 75 | 78 | 3.5 |
The horizontally grouped bar chart visually conveys the exact numbers in a narrative. For each month along the y-axis (January through June), there are 5 side-by-side colored bars, each corresponding to one of the metrics (average weight gain, follow-up rate, patient satisfaction, medication adherence, and readmission rate), and each extends from 0 to 90 on the x-axis.
This way, we can straight away compare, in a given month, how average weight gain (the shortest bars) compares to follow-up rate, patient satisfaction, medication adherence, and readmission rate (longer bars to the right) (see Figure 1). Over the course of six months, the incremental increase in the length of most bars indicates steady improvement; patient satisfaction and medication adherence increase most significantly after March; and the Readmission Rate bars decrease from month to month, visually depicting a decreasing readmission rate.
While the spreadsheet provides exact numbers for a thorough review, the bar graph provides a clear, at-a-glance illustration of these five. It is easy to identify both positive trends (e.g., increased adherence and satisfaction) and the corresponding drop in readmission rates.
Figure 1: Healthcare Outcome Trends by Month
Conclusions and Recommendations
Based on these findings, several recommendations are suggested. First, to increase the use of predictive analytics to include other data streams (social determinants of health, for example) to help further refine risk stratification models. Second, to create patient education modules in the EHR system to automatically tailor patient discharge instructions to individual patient risk profiles.
Third, implement multidisciplinary care huddles twice per week to review flagged high-risk patients and ensure accountability for follow-up and timely resource allocation. Fourth, use telehealth platforms for weight monitoring and medication counseling, especially for patients in remote and underserved areas (Anawade et al., 2024).
Finally, formalize a quarterly review process to benchmark against regional and national standards, using a balanced scorecard with clinical, financial, and patient-reported outcomes. These recommendations align with CMS’s integrated care model, which underscores that data-driven, collaborative interventions are sustainable pathways to long-term quality improvement.
Rationale for Data Collection Methods: The proposed methods for collecting information are vital for identifying the factors that lead to people with heart failure being readmitted to the hospital. Using EHR extraction provides reliable, real-time data on when patients are discharged and whether they are readmitted, helping track their overall outcomes (Brown et al., 2022).
Predictive analytics enables early identification of high-risk patients by analyzing their clinical data, such as weight gain, which could indicate fluid retention in people with heart failure. Self-reports from patients and their pharmacy refill history help determine how closely they adhere to their medication regimen, which plays a significant role in reducing hospital readmissions. Also, using patient satisfaction surveys, it is possible to continuously measure the quality of care and engagement, so we can improve care as needed quickly.
Explore Next Assessment: NURS FPX 6424 Assessment 4
Need help with NURS FPX 6224 Assessment 3? Tutors Academy provides proven strategies to improve grades quickly and confidently!
Step-By-Step Instructions To Write NURS FPX 6424 Assessment 3
Contact us to receive step-by-step instructions to write this assessment.
Instructions file for 6424 Assessment 3
Contact us to get the instruction file.
Scoring Guide for 6424 Assessment 3
Contact us to get the scoring guide.
References For
NURS FPX 6424 Assessment 3
Anawade, P. A., Sharma, D., & Gahane, S. (2024). A comprehensive review of exploring the impact of telemedicine on healthcare accessibility. Cureus, 16(3). https://doi.org/10.7759/cureus.55996
Baryakova, T. H., Pogostin, B. H., Langer, R., & McHugh, K. J. (2023). Overcoming barriers to patient adherence: The case for developing innovative drug delivery systems. Nature Reviews. Drug Discovery, 22(5), 387–409. https://doi.org/10.1038/s41573-023-00670-0
Brown, J. R., Ricket, I. M., Reeves, R. M., Shah, R. U., Goodrich, C. A., Gobbel, G., Stabler, M. E., Perkins, A. M., Minter, F., Cox, K. C., Dorn, C., Denton, J., Bray, B. E., Gouripeddi, R., Higgins, J., Chapman, W. W., MacKenzie, T., & Matheny, M. E. (2022). Information extraction from electronic health records to predict readmission following acute myocardial infarction: Does natural language processing using clinical notes improve prediction of readmission? Journal of the American Heart Association, 11(7). https://doi.org/10.1161/jaha.121.024198
Cui, J., Du, J., Zhang, N., & Liang, Z. (2025). National patient satisfaction survey as a predictor for quality of care and quality improvement – experience and practice. Patient Preference and Adherence, 19, 193–206. https://doi.org/10.2147/PPA.S496684
NURS FPX 6424 Assessment 3 Proposal to Administration: Spreadsheet and Video Presentation
Macchio, P., Farrell, L., Kumar, V., Illyas, W., Barnes, M., Patel, H., Silverman, A. L., Hong Le, T., Siddique, H., Raminfard, A., Tofano, M., Sokol, J., Haggerty, G., Kaell, A., Rabbani, S., & Faro, J. (2020). 30-day readmission prevention program in heart failure patients (RAP-HF) in a community hospital: Creating a task force to improve performance in achieving CMS target goals. Journal of Community Hospital Internal Medicine Perspectives, 10(5), 413–418. https://doi.org/10.1080/20009666.2020.1800910
Pham, S. T., Nguyen, T. A., Tran, N. M., Cao, H. T. K., Le, K. K., Duong, C. X., Nguyen, T. H., Taxis, K., Dang, K. D., Nguyen, T., Pham, S. T., Nguyen, T. A., Tran, N. M., Cao, H. T. K., Le, K. K., Duong, C. X., Nguyen, T. H., Taxis, K., Dang, K. D., & Nguyen, T. (2022). Medication adherence in cardiovascular diseases. In Novel Pathogenesis and Treatments for Cardiovascular Disease. IntechOpen. https://doi.org/10.5772/intechopen.108181
Sutton, R. T., Pincock, D., Baumgart, D. C., Sadowski, D. C., Fedorak, R. N., & Kroeker, K. I. (2020). An overview of clinical decision support systems: Benefits, risks, and strategies for success. Nature Partner Journals Digital Medicine, 3, 17. https://doi.org/10.1038/s41746-020-0221-y
Capella Professors To Choose From For NURS-FPX6424 Class
Buddy Wiltcher.
Diane Cousert.
Daphne Crenshaw.
Lisa Cox.
Kelly Salvatore.
(FAQs) related to
NURS FPX 6424 Assessment 3
Question 1: Where can I download the complete assessment for NURS FPX 6424 Assessment 3?
Answer 1: You can download the complete NURS FPX 6424 Assessment 3 from tutorsacademy.co.
Question 2: What is NURS FPX 6424 Assessment 3 Proposal to Administration: Spreadsheet and Video Presentation?
Answer 2: NURS FPX 6424 Assessment 3 is a proposal presenting heart failure readmission data analysis using a spreadsheet and video presentation.
Do you need a tutor to help with this paper for you with in 24 hours
- 0% Plagiarised
- 0% AI
- Distinguish grades guarantee
- 24 hour delivery